Lidocaine and its analogues in emergency care. Intravenous and intramuscular injections of the drug lidocaine for cardiac arrhythmias Arrhythmia and low blood pressure - what to do
1. Antiarrhythmic effect - suppresses the formation of impulses in ectopic foci of the ventricular muscles and, to a lesser extent, the atrial
2. Suppresses slightly or does not change atrioventricular and intra-triventricular conduction
H. Not in therapeutic doses inhibits myocardial contractility or inhibits it slightly. In general, the negative inotropic effect of lidocaine is much weaker than that of quinidine and procainamide.
4. Lidocaine, unlike quinidine and procainamide, with intravenous administration has no hypotensive effect
Indications. Lidocaine is used to treat ventricular extrasystoles and ventricular tachycardia in the following conditions:
For myocardial infarction
For mechanical irritation of the heart, during heart surgery and diagnostic procedures such as catheterization and angiography For intoxication with digitalis preparations After electric pulse treatment For myocarditis and other heart diseases
The effectiveness of lidocaine reaches 80% for ventricular extrasystoles and tachycardias. Lidocaine replaced procainamide as the first medicine in the treatment of ventricular tachycardia. It should be borne in mind that there are also ventricular tachycardias resistant to lidocaine, which can be affected by procainamide. However, the opposite possibility is observed much more often.
Not all ventricular extrasystoles can be treated with lidocaine. Predominantly ventricular extrasystoles are indicated for this treatment in case of myocardial infarction, mechanical irritation, intoxication with digitalis preparations, cardiopathy and when they are frequent, more than five per minute, polytopic, grouped and early, with the R-on-T phenomenon. Lidocaine is used as a prophylactic after successful electropulse treatment ventricular tachycardia and ventricular fibrillation. It is suitable for the treatment of ventricular fibrillation, resistant to electrical pulse treatment, and for the treatment of ventricular fibrillation due to intoxication with digitalis preparations.
The effect of lidocaine in the treatment of supraventricular tachycardia and extrasystoles is unreliable, so it is rarely used in such cases.
Contraindications
1. Second degree atrioventricular block and complete atrioventricular block
2. Sinoauricular block and bradycardia with escape nodal rhythm and atrioventricular dissociation
3. Severe heart failure and hypotension, when not associated with ventricular arrhythmia
4. Excessive sensitivity to local anesthetics amide series
Dosage and method of application. Lidocaine is metabolized in the liver (90%) and only a small amount is excreted unchanged from the body in the urine. Lidocaine is quickly inactivated in the body - its half-life is about 20 minutes. Lidocaine is administered intravenously under electrocardiogram control. A single dose is 50-100 mg(2% solution 2.5-5 ml), which corresponds to an average of 1-2 mg per kg of weight. The infusion is performed slowly over 1-2 minutes. The effect occurs quickly - after 1-2 minutes, and reaches a maximum after 10 minutes. The prolonged action of lidocaine is 15-20 minutes. If necessary, a single dose of lidocaine can be administered repeatedly and, sometimes, a third time at intervals of 10-15 minutes, but not more than 300 mg per hour. In patients with severe myocardial damage, heart failure, shock and liver failure, the single dose should be reduced to 25 mg. After the initial fluid injection, it is necessary to ensure slow drip introduction. For this purpose, 500 mg of lidocaine (10%-5 ml) is dissolved in 500 ml of 5% glucose solution, saline solution, Ringer's solution or dextran. The infusion rate for adults is usually 20-40, with the exception of up to 80 drops per minute, that is, 2-4 mg per minute. General daily dose 2-3 g. Drip infusion is carried out for 1-2 days, rarely more. If there are electrocardiographic signs of exceeding the dosage of lidocaine, namely prolongation of the PQ and (or) QRS interval, the rate of administration should be reduced or the infusion should be stopped for 10-25 minutes. The effective concentration of lidocaine in the blood varies from 1.5 to 2 mg per liter. At intramuscular injection of 300 mg lidocaine, apparently, it is possible to achieve 10-15 minutes after injection a satisfactory therapeutic concentration in the blood, which lingers for about two hours, without causing the risk of necrosis, in the muscle at the injection site. They prefer to inject lidocaine into the deltoid muscle. Intramuscular administration can be repeated at intervals of 3-4 hours 3-4 times a day. Lidocaine is broken down primarily in the liver. In view of this, in case of severe liver failure, it is necessary to reduce the dose of lidocaine. This must also be done in patients with renal failure and severe cardiac and peripheral vascular insufficiency.
Dosage form: solution for intravenous administration; injection Compound:Solution for intravenous administration: active substance: 2 ml of solution contains 200 mg of anhydrous lidocaine hydrochloride (in the form of lidocaine hydrochloride monohydrate 213.31 mg); excipients: water for injection
Injection: active substance: 2 ml of solution contains 40 mg of anhydrous lidocaine hydrochloride (in the form of lidocaine hydrochloride monohydrate 43 mg), excipients: sodium chloride for parenteral dosage forms, water for injections.
Description: Transparent colorless or almost colorless water solution without smell. Pharmacotherapeutic group:Local anesthetic, antiarrhythmic agent ATX:N.01.B.B Amides
N.01.B.B.02 Lidocaine
C.01.B.B.01 Lidocaine
C.01.B.B Class Ib antiarrhythmic drugs
Pharmacodynamics:According to its chemical structure, lidocaine is an acetanilide derivative. It has a pronounced local anesthetic and antiarrhythmic (lb class) effect. The local anesthetic effect is due to inhibition of nerve conduction due to blockade of sodium channels in nerve endings and nerve fibers. In its anesthetic effect it is significantly (2-6 times) superior to; the effect of lidocaine develops faster and lasts longer - up to 75 minutes, and when used simultaneously with epinephrine - more than 2 hours. At local application dilates blood vessels and does not have a local irritating effect.
The antiarrhythmic properties of lidocaine are due to its ability to stabilize the cell membrane, block sodium channels, and increase membrane permeability for potassium ions. With virtually no effect on the electrophysiological state of the atria, it accelerates repolarization in the ventricles, inhibits the fourth phase of depolarization in Purkinje fibers (diastolic depolarization phase), reducing their automaticity and the duration of the action potential, and increases the minimum potential difference at which myofibrils respond to premature stimulation. The rate of rapid depolarization (phase 0) is not affected or slightly reduced. It does not have a significant effect on the conductivity and contractility of the myocardium (it inhibits conductivity only in large, close to toxic doses). The PQ, QRS and QT intervals do not change under its influence on the ECG. Negative inotropic effect is also slightly expressed and appears short-term only with rapid administration of the drug in large doses.
Pharmacokinetics:Time to reach maximum plasma concentration after intramuscular injection- 5-15 minutes, at low speed intravenous infusion without an initial saturating dose - after 5-6 hours (in patients with acute myocardial infarction - up to 10 hours). Blood plasma proteins bind 50 - 80% of the drug. Quickly distributed (T1/2 distribution phase - 6-9 minutes) in organs and tissues with good perfusion, incl. in the heart, lungs, liver, kidneys, then in muscle and adipose tissue. Penetrates the blood-brain and placental barriers and is secreted into breast milk (up to 40% of the concentration in maternal plasma). Metabolized mainly in the liver (90-95% of the dose) with the participation of microsomal enzymes with the formation of active metabolites - glycine xylidide monoethylglycine xylidide, having a half-life of 2 hours and 10 hours, respectively. Metabolic intensity decreases in liver diseases (can range from 50 to 10% of the normal value); in case of impaired liver perfusion in patients after myocardial infarction and/or with congestive heart failure. The half-life of continuous infusion for 24-48 hours is about 3 hours; if renal function is impaired, it can increase 2 or more times. Excreted in bile and urine (up to 10% unchanged). Acidification of urine increases the excretion of lidocaine. Indications:Infiltration, conduction, spinal and epidural anesthesia. Terminal anesthesia (including in ophthalmology).
Relief and prevention of repeated ventricular fibrillation in acute coronary syndrome and repeated paroxysms of ventricular tachycardia (usually within 12-24 hours).
Ventricular arrhythmias caused by glycoside intoxication.
Contraindications:Sick sinus syndrome; severe bradycardia; atrioventricular block II- III degree(except when a ventricular stimulation probe is inserted); sinoatrial blockade, WPW syndrome, acute and chronic heart failure (III-IV F.K.); cardiogenic shock; pronounced decrease blood pressure, Adams-Stokes syndrome; intraventricular conduction disorders
Hypersensitivity to any of the components of the drug;
Retrobulbar administration to patients with glaucoma;
Pregnancy, breast-feeding(penetrates the placental barrier and is excreted in breast milk).
Carefully:Chronic heart failure II-III degree, arterial hypotension, hypovolemia, atrioventricular block I degree, sinus bradycardia, severe hepatic and/or renal failure, myasthenia gravis, epileptiform seizures (including a history), reduced hepatic blood flow, debilitated or elderly patients (over 65 years of age), children under 18 years of age (due to slow metabolism, accumulation of the drug is possible) , history of hypersensitivity to other amide local anesthetics.
It is also necessary to consider general contraindications to conduct one or another type of anesthesia.
Directions for use and dosage:For infiltration anesthesia: intradermal, subcutaneous, intramuscular. Apply lidocaine solution 5 mg/ml (maximum dose 400 mg)
For the blockade peripheral nerves And nerve plexuses : perineural, 10-20 ml of a solution of 10 mg/ml or 5-10 ml of a solution of 20 mg/ml (no more than 400 mg).
For conduction anesthesia : solutions of 10 mg/ml and 20 mg/ml (no more than 400 mg) are used perineurally.
For epidural anesthesia: epidural, solutions 10 mg/ml or 20 mg/ml (not more than 300 mg).
For spinal anesthesia: subarachnoid, 3-4 ml of a solution of 20 mg/ml (60-80 mg).
In ophthalmology: a solution of 20 mg/ml is instilled into the conjunctival sac, 2 drops 2-3 times with an interval of 30-60 seconds immediately before surgical intervention or research.
To prolong the effect of lidocaine, it is possible to add ex tempore 0.1% adrenaline solution (1 drop per 5-10 ml of lidocaine solution, but no more than 5 drops for the entire volume of the solution).
As an antiarrhythmic agent: intravenously. Lidocaine solution for intravenous administration 100 mg/ml can only be used after dilution! 25 ml of a 100 mg/ml solution should be diluted with 100 ml of saline to a lidocaine concentration of 20 mg/ml. This diluted solution is used to administer the loading dose. Administration begins with a loading dose of 1 mg/kg (over 2-4 minutes at a rate of 25-50 mg/min) followed immediately by a continuous infusion at a rate of 1-4 mg/min. Due to rapid distribution (half-life approximately 8 minutes), 10-20 minutes after the first dose, the concentration of the drug in the blood plasma decreases, which may require repeated bolus administration (against the background of continuous infusion) at a dose equal to 1/2-1/3 loading dose, with an interval of 8-10 minutes.
Maximum dose at 1 hour - 300 mg, per day - 2000 mg.
The intravenous infusion is usually given for 12 to 24 hours with continuous ECG monitoring, after which the infusion is stopped to assess the need for changes in the patient's antiarrhythmic therapy.
The rate of drug elimination is reduced in heart failure and liver dysfunction (cirrhosis, hepatitis) and in elderly patients, which requires a reduction in the dose and rate of drug administration by 25-50%.
For chronic renal failure no dose adjustment is required.
Side effects:From the outside nervous system, sense organs:euphoria, headache, dizziness, drowsiness, general weakness, neurotic reactions, confusion or loss of consciousness, disorientation, convulsions, tinnitus, paresthesia, diplopia, nystagmus, photophobia, tremor, trismus of facial muscles, anxiety.
From the outside of cardio-vascular system: decreased blood pressure, peripheral vasodilation, collapse, chest pain, bradycardia (up to cardiac arrest).
Allergic reactions: skin rash, urticaria, itching, angioedema, anaphylactic shock.
From the outside digestive system: nausea, vomiting.
Other:sensation of “hot” or “cold”, persistent anesthesia, erectile dysfunction, hypothermia, methemoglobinemia.
Overdose:Symptoms: the first signs of intoxication - dizziness, nausea, vomiting, euphoria, decreased blood pressure, asthenia; then - convulsions of facial muscles with transition to tonic-clonic convulsions of skeletal muscles, psychomotor agitation, bradycardia, asystole, collapse; when used during childbirth in a newborn - bradycardia, depression respiratory center, apnea.
Treatment: cessation of drug administration, oxygen inhalation. Symptomatic therapy. For convulsions, 10 mg of diazepam is administered intravenously. For bradycardia - m-anticholinergic blockers (), vasoconstrictors (,). Hemodialysis is ineffective.
Interaction:Beta blockers also increase the risk of toxic effects.
Reduces the cardiotonic effect of digitoxin.
Enhances muscle relaxation of curare-like drugs.
Ajmaline, and enhance the negative inotropic effect. Inducers of microsomal liver enzymes (barbiturates) reduce the effectiveness of lidocaine.
Vasoconstrictors (methoxamine) prolong the local anesthetic effect of lidocaine and can cause increased blood pressure and tachycardia.
Lidocaine reduces the effect of antimyasthenic drugs.
Concomitant use with procainamide can cause stimulation of the central nervous system and hallucinations.
Guanadrel, guanethidine, mecamylamine, trimethaphan increase the risk of a pronounced decrease in blood pressure and bradycardia. Strengthens and prolongs the effect of muscle relaxants.
The combined use of lidocaine and phenytoin should be used with caution, as it is possible to reduce the resorptive effect of lidocaine, as well as the development of an undesirable cardiodepressive effect.
Under the influence of monoamine oxidase inhibitors, the local anesthetic effect of lidocaine and a decrease in blood pressure are likely to be enhanced. Patients taking monoamine oxidase inhibitors should not be administered parenterally.
When lidocaine and polymykisin B are prescribed simultaneously, it is necessary to monitor the patient's respiratory function.
When lidocaine is used in combination with hypnotics or sedatives, narcotic analgesics, hexenal or sodium thiopental, the inhibitory effect on the central nervous system and respiration may be enhanced.
When lidocaine is administered intravenously to patients taking it, undesirable effects such as a state of stupor, drowsiness, bradycardia, paresthesia, etc. are possible. This is due to an increase in the level of lidocaine in the blood plasma, which is explained by the release of lidocaine from binding to blood proteins, as well as a slowdown in its inactivation in the liver. If combination therapy with these drugs is necessary, the dose of lidocaine should be reduced.
When treating the injection site with disinfectant solutions containing heavy metals, the risk of developing local reaction in the form of pain and swelling.
Special instructions:It is necessary to discontinue MAO inhibitors at least 10 days in case of planned use of lidocaine.
Caution should be exercised when performing local anesthesia in highly vascularized tissues; aspiration testing is recommended to avoid intravascular injection.
Impact on the ability to drive vehicles. Wed and fur.:During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions. Release form/dosage:Solution for intravenous administration 100 mg/ml. Package: 2 ml of the drug in colorless glass ampoules of hydrolytic class I with two code rings (red and green) and a white break line. 5 ampoules per blister pack. 2 blister packs each along with instructions for medical use placed in a cardboard box. Solution for injection 20 mg/ml. 2 ml per ampoule with a notch and a green code ring, 5 ampoules in a blister pack sealed with transparent PE film, 20 blister packs per cardboard box sealed with a label along with instructions for use. Storage conditions:At a temperature of 15 to 25°C, out of the reach of children. Best before date: 5 years. Do not use after the expiration date indicated on the package. Conditions for dispensing from pharmacies: On prescription Registration number: P N014235/03 Registration date: 26.09.2008 Expiration date: Indefinite Owner Registration certificate: Hungary Manufacturer: Representative office: EGIS CJSC pharmaceutical plant Hungary Information update date: 26.02.2018 Illustrated instructionsCompound
1 tablet contains the active substance: lidocaine hydrochloride monohydrate 20 mg (in terms of lidocaine hydrochloride 100 mg).
Pharmacotherapeutic group
Local anesthetic, antiarrhythmic agent.
ATX code
N01BB02, С01ВВ01
pharmachologic effect
According to its chemical structure, lidocaine is an acetanilide derivative. It has a pronounced local anesthetic and antiarrhythmic (class 1b) effect. The local anesthetic effect is due to inhibition of nerve conduction due to the blockade of sodium channels in nerve endings and nerve fibers. In its anesthetic effect, lidocaine is significantly (2-6 times) superior to procaine; the effect of lidocaine develops faster and lasts longer - up to 75 minutes, and when used simultaneously with epinephrine - more than 2 hours. When applied topically, it dilates blood vessels and does not have a local irritating effect. The antiarrhythmic properties of lidocaine are due to its ability to stabilize the cell membrane, block sodium channels, and increase membrane permeability for potassium ions. With virtually no effect on the electrophysiological state of the atria, lidocaine accelerates repolarization in the ventricles, inhibits phase IV depolarization in Purkinje fibers (phase of diastolic depolarization), reducing their automaticity and the duration of the action potential, and increases the minimum potential difference at which myofibrils respond to premature stimulation. The rate of rapid depolarization (phase 0) is not affected or slightly reduced. It does not have a significant effect on the conductivity and contractility of the myocardium (it inhibits conductivity only in large, close to toxic doses). The PQ, QRS and QT intervals do not change under its influence on the ECG. The negative inotropic effect is also slightly expressed and appears short-term only with rapid administration of the drug in large doses.
Indications for use
Infiltration, conduction, spinal and epidural anesthesia. Terminal anesthesia in ophthalmology. Prevention of repeated ventricular fibrillation in acute coronary syndrome and repeated paroxysms of ventricular tachycardia (usually within 12-24 hours). Ventricular arrhythmias caused by glycoside intoxication.
Contraindications
Hypersensitivity to amide-type local anesthetics or any excipient drug. Sick sinus syndrome, severe bradycardia, atrioventricular block II-III degree (except when a probe is inserted to stimulate the ventricles), Wolff-Parkinson-White syndrome, acute and chronic heart failure (III-IV functional class), cardiogenic shock, Morgagni-Adams-Stokes syndrome, intraventricular conduction disorders, sinoatrial block, cardiogenic shock. Infection of the intended injection site. Retrobulbar administration to patients with glaucoma. Lidocaine should not be used for epidural anesthesia in patients with severe hypotension or cardiogenic or hypovolemic shock. It is also necessary to take into account general contraindications to this or that type of anesthesia.
Directions for use and doses
For infiltration anesthesia, a 0.5% solution of lidocaine (maximum dose 400 mg) is used to block peripheral nerves and nerve plexuses, 10-20 ml of a 1% solution or 5-10 ml of a 2% solution (no more than 400 mg). for conduction anesthesia, 1% and 2% solutions are used (no more than 400 mg). for epidural anesthesia 1% and 2% solutions (not more than 300 mg). for spinal anesthesia - 3-4 ml of 2% solution (60-80 mg). in ophthalmology: a 2% solution is instilled into the conjunctival sac, 2 drops 2-3 times at intervals of 30-60 seconds, immediately before surgery or examination. To prolong the action of lidocaine, it is possible to add ex tempore 0.1% epinephrine solution (1 drop per 5-10 ml of lidocaine solution, but not more than 5 drops for the entire volume of the solution). It is recommended to reduce the dose of lidocaine in elderly patients and patients with liver diseases (cirrhosis, hepatitis) or with reduced hepatic blood flow (chronic heart failure) by 40 - 50%. as an antiarrhythmic agent: intravenously, 25 ml of a 10% solution should be diluted with 100 ml of 0.9% sodium chloride solution to a lidocaine concentration of 20 mg/ml. This diluted solution is used to administer the loading dose. Administration begins with a loading dose of 1-1.5 mg/kg (over 2-4 minutes at a rate of 25-50 mg/min) with immediate connection to a continuous infusion at a rate of 1-4 mg/min. Due to rapid distribution (half-life approximately 8 minutes), 10-20 minutes after the first dose, the concentration of the drug in the blood plasma decreases, which may require repeated bolus administration (against the background of continuous infusion) at a dose equal to 1/2-1/3 loading dose, with an interval of 8-10 minutes. The maximum dose in 1 hour is 300 mg, per day - 2000 mg. The intravenous infusion is usually given for 12 to 24 hours with continuous ECG monitoring, after which the infusion is stopped to assess the need for changes in the patient's antiarrhythmic therapy. The rate of drug elimination is reduced in case of heart failure and liver dysfunction (cirrhosis, hepatitis), which requires a reduction in the dose and rate of drug administration by 25-50%. For chronic renal failure, no dose adjustment is required.
Release form
Solution for injection 20 mg/ml and 100 mg/ml. 2 ml in ampoules of colorless neutral glass type I with a colored break ring or with a colored dot and a notch or without a break ring, a colored dot and notch. The ampoules may additionally be coated with one, two or three color rings and/or a two-dimensional barcode, and/or alphanumeric coding, or without additional color rings, a two-dimensional barcode, or alphanumeric coding. 5 ampoules per blister pack made of polyvinyl chloride film and lacquered aluminum foil or polymer film or without foil and without film. Or 5 ampoules in a pre-made form (tray) made of cardboard with cells for placing ampoules. 1, 2 or 5 blister packs or cardboard trays together with instructions for use and a scarifier or ampoule knife, or without a scarifier and ampoule knife in a cardboard package (pack).
From this article you will learn: what antiarrhythmic drugs exist, which medications are best suited in each specific case of arrhythmia.
Drug treatment of arrhythmia is the main method of treating this disease. In 90–95%, antiarrhythmic drugs can either completely eliminate arrhythmia or reduce its severity. They are equally effective in both emergency care, and with a systematic approach aimed at preventing repeated rhythm disturbances. But in order to achieve maximum treatment results, it is important to know which drugs should be used in certain cases.
Below is a list of the most effective and safe medications that are most commonly used to treat cardiac arrhythmias (in order of decreasing effectiveness):
- Potassium channel blockers - Amiodarone (its analogues Cordarone, Aritmil).
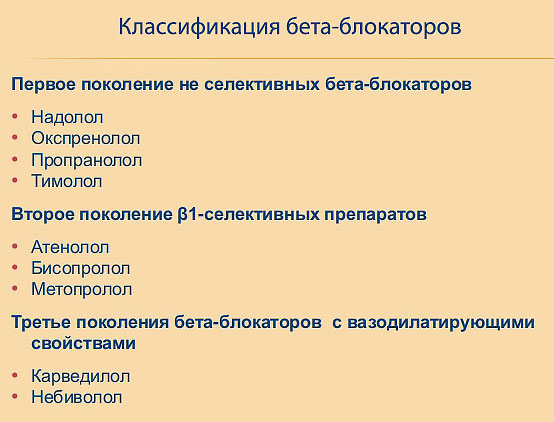
- Beta blockers – Metoprolol (Corvitol), Bisoprolol (Concor), Nebivalol.
- Calcium channel blockers – Verapamil (Isoptin, Finoptin).
- Local anesthetics – Lidocaine, Novocainamide.
- Drugs of different groups:
- cardiac glycosides - Strophanthin, Korglykon, Digoxin;
- medicines containing potassium - Panangin, Asparkam.
The selection, prescription of antiarrhythmic drugs and monitoring their effectiveness are carried out by a cardiologist, but also by a general practitioner and family doctor.
Amiodarone is a universal first-line drug
Among all drugs for the treatment of arrhythmia, amiodarone is considered the number one treatment for any heart rhythm disturbances. It is equally suitable for use in emergency mode, when the patient urgently needs to relieve an attack, and for maintenance treatment, preventing repeated heartbeat interruptions.
In what cases is it most effective: indications
Classic indications for amiodarone:
- atrial fibrillation;
- atrial fibrillation and flutter;
- supraventricular and ventricular extrasystole;
- severe sinus tachycardia (paroxysmal);
- Wolff-Parkinson-White syndrome.
Release forms and analogue drugs
Amiodarone is both an active substance and medication. There are analogues - antiarrhythmic drugs containing an identical base, but having a different name. Two medications are mainly used:
- Cordaron,
- Arhythmil.

Both amiodarone and its analogues are available in the form of tablets and solution for injection (intravenous injections).
Features of the action and advantages of the drug
Amiodarone has a unique mechanism of action - it blocks the channels through which potassium ions are transported into the heart. Due to this, the overall exchange of electrolytes, primarily sodium and calcium, slows down. Against this background, the excitability of the myocardium and the conduction system of the heart decreases - impulses for contraction occur less frequently and their conductivity decreases.
The main advantage of amiodarone is its antianginal effect. This means that the drug improves blood supply to the myocardium by reducing the need for oxygen and direct expansion coronary arteries.
- If a person has an episode of fast, irregular heartbeat, amiodarone can be given regardless of what type of arrhythmia it is.
- Due to its antianginal effect, amiodarone is the drug of choice for severe arrhythmias combined with coronary disease heart, hypertrophy and decreased contractility of the left ventricle, heart failure.
- Such antiarrhythmic drugs act slowly but for a long time, while injectable drugs, on the contrary, act quickly but for a short time. Therefore, to quickly stop attacks of arrhythmia and for several days after it, it is better to administer amiodarone intravenously (dropper or slow injection), and it is better to maintain a constant concentration of the active substance in the blood with tablets.
- Due to the strong inhibitory effect on the heart, it is contraindicated when arrhythmias are combined with conduction disorders (atrioventricular block).
- It does not affect blood pressure levels, therefore it is the only means of helping patients with arrhythmias accompanied by a decrease in blood pressure or myocardial infarction.
- The drug is well tolerated and side effects occur rarely, which makes it possible for frequent and prolonged use.
The only problem
Amiodarone does not have a sufficient therapeutic antiarrhythmic effect to relieve ventricular fibrillation and other severe ventricular arrhythmias. In such cases, preference is given to local anesthetics - Lidocaine and Novocainamide.
 Sinus rhythm of the heart on an ECG: different kinds ventricular fibrillation
Sinus rhythm of the heart on an ECG: different kinds ventricular fibrillation
Beta blockers: how to use them correctly
The point of prescribing beta blockers for arrhythmias lies in the mechanism of their action on the heart. These drugs bind to beta group receptors, through which adrenaline exerts its stimulating effects on the myocardium - it increases the frequency of contractions. By blocking the receptors with medications, this effect can be eliminated, which is important in the treatment of arrhythmia.
The most common medications in this group are Metoprolol and Bisoprolol. Compared to Amiodarone, as the standard antiarrhythmic drug, they are weaker, but in some cases they cannot be avoided. It's connected with additional effects– expansion of the coronary arteries and a decrease in blood pressure. Therefore, any beta blockers are considered the drugs of choice for a combination of mild supraventricular and atrial fibrillation, ventricular extrasystoles with:
- hypertension;
- coronary heart disease;
- disorders of cerebral circulation.
What is good about Metoprolol?
The advantage of Metoprolol (the name of the analogue is Corvitol), which makes it one of the main drugs for first aid for arrhythmias, is the fairly rapid onset of the therapeutic effect - even if such arrhythmia tablets are used. Active substance when taken under the tongue, it accumulates in the blood in a therapeutic concentration within 30–40 minutes. Therefore, it is mainly used to relieve attacks and in the immediate period after it.
Why Bisoprolol
The medicine for cardiac arrhythmia Bisoprolol (list of analogues: Concor, Biprolol) acts slowly, gradually, but for a long time (about 12 hours). This feature, combined with the pronounced effects characteristic of beta blockers, allows the drug to be used for long-term treatment and prevention of repeated cardiac arrhythmias.

Disadvantages of beta blockers
Antiarrhythmic drugs beta blockers should not be prescribed for the treatment of arrhythmias in patients:
- Chronic obstructive pulmonary diseases and bronchial asthma.
- For low blood pressure. This is very important, since about 50% of heart attacks and 20% of arrhythmic attacks are accompanied by a similar disorder.
- Severe heart failure.
- There are no injectable forms of drugs.
 Click on photo to enlarge
Click on photo to enlarge
Verapamil is an ideal drug for supraventricular arrhythmia
The mechanism of the antiarrhythmic action of Verapamil is associated with a slowdown in the transport of calcium ions into the heart. Thereby:
- the excitability of the myocardium and conduction system decreases;
- contraction frequency decreases;
- general blood pressure decreases.
The key feature is that cardiac effects are expressed exclusively in the supraventricular zone - the atria and sinus node. Therefore, Verapamil and its analogues (Isoptin, Finoptin) are mainly used for atrial fibrillation and fibrillation, supraventricular extrasystoles. It is especially relevant if such arrhythmias are combined with increased blood pressure or angina pectoris.
It is available both in the form of an injection solution for intravenous administration, which is convenient for eliminating an attack, and in tablets, which allows it to be used to prevent relapse.

Local anesthetics - when to use them
Drugs for local anesthesia (Lidocaine and Novocainamide) in addition to the anesthetic effect have an antiarrhythmic effect. It is most pronounced in relation to the ventricles of the heart. None of existing funds for the treatment of arrhythmia does not have a similar effect.
Both Novocainamide and Lidocaine are available only in injection form. They are administered intravenously in exceptional cases for ventricular arrhythmias - ventricular fibrillation and fibrillation, frequent ventricular extrasystoles. They act immediately after administration, but only for a short time. They are effective, but not without side effects in the form of allergic reactions.

Auxiliary drugs that help with arrhythmia
For mild attacks of atrial fibrillation, paroxysmal tachycardia, supraventricular and ventricular extrasystole, a sufficient therapeutic effect can be obtained from:
- preparations containing potassium and magnesium ions - Aspacam, Panangin;
- cardiac glycosides - Strophanthin, Korglykon, Digoxin.
For emergency treatment both are administered intravenously: Asparkam and Panangin drip, and glycosides in a stream (slow intravenous injection). The mechanism of action is associated with slowing the transport of sodium ions into cells, reducing its excitability and increasing contractility. These drugs are also available in tablets, but their antiarrhythmic effect is weakly expressed, more so with long-term use.
Even if you know the names of the drugs, this does not give you the right to use antiarrhythmic drugs without the advice of a specialist!
Intravenous and intramuscular injections of the drug Lidocaine for cardiac arrhythmias

This medicine used to restore normal heart rhythm in all types of ventricular arrhythmias. Lidocaine is recommended for myocardial infarction, as well as an overdose of cardiac glycosides. The drug is administered intravenously as a stream in acute conditions, then as part of droppers or intramuscularly.
Read in this article
Action in case of rhythm disturbance
The antiarrhythmic properties of Lidocaine manifest themselves mainly at the level of ventricular myocardial cells in the form of the following biological reactions:
- stabilizes the membrane;
- improves potassium penetration;
- accelerates recovery after the passage of an impulse;
- inhibits the process of excitation in Purkinje fibers;
- reduces the duration of the active period;
- stops the circular circulation of the signal.
It should also be taken into account that the point of application for Lidocaine is the cells of the conduction system of the heart, which are located directly in the ventricles. For atrial arrhythmias, prescribing medication is not advisable.
In therapeutic doses, Lidocaine solution does not disrupt the conduction of impulses and the force of myocardial contraction. When large quantities of the drug are administered rapidly, these adverse reactions may still occur, but a short time. When entering a vein, the onset of action occurs “at the tip of the needle” - within one minute, and lasts about 20 minutes. Intramuscular injections normalize the rhythm in 5 - 10 minutes, their effect lasts up to 1.5 hours.
And here is more information about the treatment of ventricular tachycardia.
Indications for use
In cardiological practice, the drug is prescribed for the following ventricular arrhythmias:
- against the background of myocardial infarction;
- attack of tachycardia;
- prevention of rhythm disturbances during heart surgery, installation of an artificial pacemaker, long-term general anesthesia;
- prevention of recurrent fibrillation;
- overdose of cardiac glycosides;
- extrasystole;
- ventricular flutter.
 Extrasystole is one of the indications for the use of lidocaine
Extrasystole is one of the indications for the use of lidocaine
Contraindications
- heavy bleeding;
- significant slowdown in heart rate;
- blockade of impulse conduction at the level of the atrioventricular node;
- pronounced manifestations of circulatory failure;
- state of shock, including cardiogenic origin;
- low blood pressure, collapse;
- liver dysfunction;
- convulsive syndrome.
For these categories of patients, the use of lidocaine is indicated for life-threatening conditions. In case of cardiovascular failure and impaired renal function, myasthenia gravis, the drug is administered under constant medical supervision. Before using this remedy, it is necessary to compensate for the deficiency of circulating blood and potassium content.
Application and dosage
To stop an attack of arrhythmia, the drug is first injected into a vein as a stream (up to 80 mg), and then in a dropper at a rate of 2 - 3 mg per minute. To carry out the infusion, you need to dilute 8 ml of 2% Lidocaine in 80 mg of 0.9% sodium chloride. The maximum amount of such a solution per day is 800 - 1000 ml.
There is another scheme for restoring rhythm:
- intravenously 4 ml of 2% solution;
- intramuscularly 2 ml 10% every 3 - 4 hours.
The total dose cannot exceed 300 mg per hour and 2000 mg per day. Lidocaine ampoules for intravenous jet administration should be only 2% concentration, and a 10% solution is used for intramuscular injections or diluted for infusion.
Watch the video about methods of treating arrhythmia:
Side effects
In the past, lidocaine was prescribed for myocardial infarction to prevent arrhythmia. Such recommendations were then revised as the risk of cardiac arrest increases. This drug has a pronounced antiarrhythmic effect, but its use should be monitored by a doctor due to the threat of complications:
- disturbances of consciousness,
- convulsions,
- change in emotional background,
- neurotic reactions,
- drowsiness,
- double vision,
- tinnitus,
- dizziness,
- spasm of facial muscles,
- trembling of limbs,
- pressure drop,
- slowing heart rate
- heartache,
- rashes,
- skin itching,
- involuntary urination,
- respiratory depression,
- difficulty speaking.
 Lidocaine can be administered with other antiarrhythmic drugs to enhance the effect - Novocainamide, Cordarone, Ornid. In this case, its dose is reduced, and toxic effect prevented.
Lidocaine can be administered with other antiarrhythmic drugs to enhance the effect - Novocainamide, Cordarone, Ornid. In this case, its dose is reduced, and toxic effect prevented.
Rapid entry into the blood is accompanied by a pronounced drop in blood pressure. In this case, Mezaton or Dopamine is indicated.
When using the drug, the ability to quickly react and concentrate is significantly reduced, so driving is prohibited for the period of treatment. Vehicle, control of mechanisms in production.
Overdose
When large quantities of the drug are administered or its elimination from the body is impaired, the following symptoms are possible:
- strong motor and mental agitation;
- general weakness;
- convulsions;
- blockade of impulse transmission through the myocardium;
- loss of consciousness;
- respiratory arrest;
- coma.
When these signs appear, the injections are stopped. Patients are given ventilation, oxygen therapy, and in the absence of spontaneous breathing, they are connected to an artificial pulmonary ventilation device. In case of cardiac arrest, resuscitation measures. Anticonvulsants and anti-anxiety medications may also be recommended.
And here is more information about arrhythmia in diabetes.
To treat heart rhythm disturbances, intravenous and intramuscular injections of lidocaine are prescribed. It normalizes the polarity of cell membranes, inhibits the circulation of pathological impulses in the ventricular myocardium. Indicated for tachycardia, extrasystole, flutter and ventricular fibrillation. It can be used by patients with a heart attack, during heart surgery, and digitalis intoxication.
Dangerous side effects require medical supervision upon introduction.

For extrasystole, atrial fibrillation, and tachycardia, drugs of both new, modern and old generation are used. The current classification of antiarrhythmic drugs allows you to quickly make a choice from groups based on indications and contraindications

Magnesium is prescribed for hypertension. Treatment is often carried out with IV drips. The course is selected by the doctor depending on the indicators and condition of the patients.

Poisoning with cardiac glycosides can occur due to various reasons. Regardless of them, the patient requires urgent assistance even before the ambulance arrives.

A polarizing mixture has been used for a long time in cardiology. Indications are: the need to reduce the area of necrosis, improve the oxygen supply to the heart, and others. It is used in various variations, including with potassium and magnesium.

You can take pills for heart palpitations only after consulting a cardiologist. The fact is that only he can choose which ones are needed to reduce the heart rate, since not all will help against a strong, rapid rhythm, tachycardia, arrhythmia.

A change in heart rhythm, which doctors call paroxysmal ventricular tachycardia, is deadly. It can be polymorphic, fusiform, bidirectional, unstable, monomorphic. What does it look like on an ECG? How to stop an attack?

Analgesics are prescribed for a heart attack to relieve acute pain and general improvement of the patient's condition. In case of myocardial infarction, narcotic painkillers, tranquilizers, opioids will help, in some cases nitrous oxide is needed.

The treatment method for ventricular tachycardia includes the use of drugs, electrical impulses, and in severe cases, the installation of a cardioverter-defibrillator. Relief of symptoms of paroxysmal VT affects the prognosis of the disease.

If the doctor prescribed Proctosan suppositories, the use will be a little uncomfortable, but effective. The composition is selected in such a way as to relieve itching and burning from hemorrhoids. Is it possible during pregnancy? When is the best time to choose an ointment?
Cardiologist - site about heart and vascular diseases
Cardiologist online
Heart surgeon online
Lidocaine
pharmachologic effect
Class IB antiarrhythmic agent, local anesthetic, acetanilide derivative. Has membrane stabilizing activity. Causes blockade of sodium channels of excitable membranes of neurons and membranes of cardiomyocytes.
This local anesthetic has antiarrhythmic properties and is used to relieve ventricular arrhythmias. Previously, lidocaine was administered to all patients with suspected myocardial infarction, and this led to a reduction in the risk of ventricular fibrillation. However, as it turned out, the mortality rate increased - perhaps
because lidocaine worsens AV block and, rarely, heart failure. Therefore, at present, from the mandatory administration of lidocaine for suspected
myocardial infarction refused.
Reduces the duration of the action potential and the effective refractory period in Purkinje fibers, suppresses their automaticity. In this case, lidocaine suppresses the electrical activity of depolarized, arrhythmogenic areas, but has minimal effect on the electrical activity of normal tissues. When used in average therapeutic doses, it practically does not change myocardial contractility and does not slow down AV conduction. When used as an antiarrhythmic drug with intravenous administration, the onset of action is 45-90 seconds, duration is 10-20 minutes; with intramuscular administration, the onset of action is 5-15 minutes, duration is 60-90 minutes.
Causes all types of local anesthesia: terminal, infiltration, conduction.
Pharmacokinetics
Lidocaine is well absorbed but undergoes significant, although variable, first-pass metabolism in the liver. In this regard, it is not prescribed internally. In principle, maintaining therapeutic concentrations is possible with regular IM injections, but the IV route of administration is preferred. The metabolism of lidocaine produces glycyl(n)xylidide and monoethylglycyl(n)xylidide, which have less activity on fast sodium channels. Glycyl(n)xylidide and lidocaine compete for binding sites on fast sodium channels, which may lead to decreased activity of lidocaine during IV infusion, accompanied by accumulation of glycyl(n)xylidide.
On the other hand, with an infusion lasting more than 24 hours, the elimination of lidocaine is reduced, apparently due to competition between lidocaine and its metabolites for liver enzymes.
The serum concentration of lidocaine decreases biexponentially after administration, so its pharmacokinetics are described by a multicompartment model.
After a single intravenous injection, the concentration of lidocaine decreases rapidly (T1/2 about 8 minutes), which reflects the distribution of the drug in the tissues. The final half-life, usually 100-120 minutes, reflects the hepatic metabolism of lidocaine.
In heart failure, the volume of distribution of lidocaine is reduced, so the saturation dose is reduced. Since the elimination of lidocaine is also reduced, it is necessary to reduce maintenance doses. In addition, the elimination of lidocaine is reduced with liver disease, taking cimetidine and beta-blockers, and
also with prolonged lidocaine infusion. In these conditions, it is necessary to regularly measure the serum concentration of lidocaine and maintain it in the therapeutic range (1.5-5 μg/ml).
Lidocaine binds to the acute phase protein alpha-1-acid glycoprotein. During myocardial infarction and other diseases, the concentration of this protein increases, which leads to a decrease in the proportion of free drug. Apparently, this is why in case of myocardial infarction, higher doses are sometimes required to achieve an antiarrhythmic effect, and patients tolerate them well.
Indications
In cardiological practice: treatment and prevention of ventricular arrhythmias (extrasystole, tachycardia, flutter, fibrillation), incl. V acute period myocardial infarction, with implantation of an artificial pacemaker, with glycoside intoxication, anesthesia.
For anesthesia: terminal, infiltration, conduction, spinal (epidural) anesthesia in surgery, obstetrics and gynecology, urology, ophthalmology, dentistry, otorhinolaryngology; blockade of peripheral nerves and nerve ganglia.
Dosage regimen
The effect of lidocaine depends on its serum concentration. Therefore, with the jet administration of lidocaine, the arrhythmia may stop, but then resume as the drug is distributed in the tissues and its serum concentration drops. To avoid this, use the following scheme. First, 3-4 mg/kg IV is administered over 20-30 minutes (for example, 100 mg, then 3 times 50 mg every 8 minutes). Next, infusion is carried out at a rate of 1-4 mg/min; this rate of administration corresponds to the rate of hepatic metabolism. The serum concentration of lidocaine reaches a steady-state level after 8-10 hours of infusion. If the maintenance infusion rate is too slow, the arrhythmia may recur several hours after the start of seemingly successful therapy. On the other hand, too rapid infusion may lead to adverse reactions. To select the correct maintenance dose, measure the serum concentration of lidocaine after the expected achievement of a steady state.
2-4 mg/kg is administered intramuscularly; if necessary, repeated administration is possible after 60-90 minutes.
For children, with intravenous administration of a loading dose - 1 mg/kg, if necessary, repeated administration after 5 minutes. For continuous IV infusion (usually after administration of a loading dose) - 20-30 mcg/kg/min.
For use in surgical and obstetric practice, dentistry, and ENT practice, the dosage regimen is set individually, depending on the indications, clinical situation and dosage form used.
Maximum doses: for adults, with intravenous administration, the loading dose is 100 mg, with subsequent drip infusion - 2 mg/min; with intramuscular administration - 300 mg (about 4.5 mg/kg) for 1 hour.
For children, in case of repeated administration of a loading dose with an interval of 5 minutes, the total dose is 3 mg/kg; with continuous intravenous infusion (usually after administration of a loading dose) - 50 mcg/kg/min.
Side effect
From the central nervous system and peripheral nervous system: dizziness, headache, weakness, motor restlessness, nystagmus, loss of consciousness, drowsiness, visual and hearing impairment, tremor, trismus, convulsions (the risk of their development increases against the background of hypercapnia and acidosis), cauda equina syndrome (leg paralysis, paresthesia), paralysis of the respiratory muscles, respiratory arrest, motor and sensory block, respiratory paralysis (more often develops with subarachnoid anesthesia ), numbness of the tongue (when used in dentistry).
With rapid intravenous administration of large doses of lidocaine, epileptic seizures may occur. If the serum concentration of lidocaine slowly increases to a toxic level (with long-term treatment), then tremor, dysarthria and disturbances of consciousness often develop. An early sign of lidocaine intoxication is nystagmus.
From the cardiovascular system: increase or decrease in blood pressure, tachycardia - when administered with a vasoconstrictor, peripheral vasodilation, collapse, chest pain.
From the digestive system: nausea, vomiting, involuntary bowel movements.
Allergic reactions: skin rash, urticaria (on the skin and mucous membranes), skin itching, angioedema, anaphylactic shock.
Local reactions: with spinal anesthesia - back pain, with epidural anesthesia - accidental entry into the subarachnoid space; when applied topically in urology - urethritis.
Other: involuntary urination, methemoglobinemia, persistent anesthesia, decreased libido and/or potency, respiratory depression, even stopping, hypothermia; during anesthesia in dentistry: insensitivity and paresthesia of the lips and tongue, prolongation of anesthesia.
Contraindications
Severe bleeding, shock, hypotension, infection of the intended injection site, severe bradycardia, cardiogenic shock, severe forms chronic heart failure, CVS in elderly patients, AV blockade of II and III degrees (except when a probe is inserted to stimulate the ventricles), severe liver dysfunction.
For subarachnoid anesthesia - complete heart block, bleeding, arterial hypotension, shock, infection of the lumbar puncture site, septicemia.
Hypersensitivity to lidocaine and other amide-type local anesthetics.
During pregnancy and lactation, use only for health reasons. Lidocaine is excreted in breast milk.
In obstetric practice, use paracervically with caution in cases of intrauterine development disorders of the fetus, fetoplacental insufficiency, prematurity, postmaturity, and gestosis.
special instructions
Caution should be used in conditions accompanied by a decrease in hepatic blood flow (including chronic heart failure, liver diseases), progressive cardiovascular failure (usually due to the development of heart block and shock), in severe and debilitated patients, in elderly patients age (over 65 years); for epidural anesthesia - for neurological diseases, septicemia, impossibility of puncture due to spinal deformity; for subarachnoid anesthesia - for back pain, brain infections, benign and malignant neoplasms brain, with coagulopathies of various origins, migraine, subarachnoid hemorrhage, arterial hypertension, arterial hypotension, paresthesia, psychosis, hysteria, in non-contact patients, impossibility of puncture due to spinal deformity.
Lidocaine solutions should be administered with caution into tissues with abundant vascularization (for example, in the neck area during operations on thyroid gland), in such cases lidocaine is used in smaller doses.
When used simultaneously with beta-blockers and cimetidine, a reduction in the dose of lidocaine is required; with polymyxin B - respiratory function should be monitored.
During treatment with MAO inhibitors, lidocaine should not be used parenterally.
Injection solutions containing epinephrine and norepinephrine are not intended for intravenous administration.
Lidocaine should not be added to blood transfusions.
Impact on the ability to drive vehicles and operate machinery
Drug interactions
When used simultaneously with barbiturates (including phenobarbital), it is possible to increase the metabolism of lidocaine in the liver, reduce the concentration in the blood plasma and, as a result, reduce its therapeutic effectiveness.
When used simultaneously with beta-blockers (including propranolol, nadolol), the effects of lidocaine (including toxic ones) may be enhanced, apparently due to a slowdown in its metabolism in the liver.
When used simultaneously with MAO inhibitors, the local anesthetic effect of lidocaine may be enhanced.
When used simultaneously with drugs that block neuromuscular transmission (including suxamethonium chloride), the effect of drugs that block neuromuscular transmission may be enhanced.
When used simultaneously with hypnotics and sedatives, the inhibitory effect on the central nervous system may be enhanced; with ajmaline, quinidine - increased cardiodepressive effect is possible; with amiodarone - cases of seizures and SSSS have been described.
When used simultaneously with hexenal, sodium thiopental (iv), respiratory depression is possible.
When used simultaneously with mexiletine, the toxicity of lidocaine increases; with midazolam - a moderate decrease in the concentration of lidocaine in the blood plasma; with morphine - enhances the analgesic effect of morphine.
When used simultaneously with prenylamine, there is a risk of developing ventricular arrhythmia of the “pirouette” type.
Cases of agitation and hallucinations have been described when used simultaneously with procainamide.
When used simultaneously with propafenone, the duration and severity of side effects from the central nervous system may increase.
It is believed that under the influence of rifampicin, a decrease in the concentration of lidocaine in the blood plasma is possible.
With simultaneous intravenous infusion of lidocaine and phenytoin, side effects of central origin may increase; a case of sinoatrial block due to the additive cardiodepressive effect of lidocaine and phenytoin is described.
In patients receiving phenytoin as an anticonvulsant, a decrease in the concentration of lidocaine in the blood plasma is possible, which is due to the induction of microsomal liver enzymes under the influence of phenytoin.
When used simultaneously with cimetidine, the clearance of lidocaine moderately decreases and its concentration in the blood plasma increases, there is a risk of increased side effect lidocaine.
Lidocaine - instructions for use, reviews, analogs and release forms (injections in ampoules for injection and dilution in solution, spray, gel or ointment 5%) of a medicinal product for the treatment of arrhythmias and pain relief in adults, children and pregnancy
In this article you can find instructions for use medicinal product Lidocaine. Reviews of site visitors - consumers of this medicine, as well as the opinions of specialist doctors on the use of Lidocaine in their practice are presented. We kindly ask you to actively add your reviews about the drug: whether the medicine helped or did not help get rid of the disease, what complications and side effects were observed, perhaps not stated by the manufacturer in the annotation. Lidocaine analogues in the presence of existing structural analogues. Use for the treatment of arrhythmias and anesthesia (pain relief) in adults, children, as well as during pregnancy and lactation.
Lidocaine- according to its chemical structure, it belongs to acetanilide derivatives. It has a pronounced local anesthetic and antiarrhythmic effect. The local anesthetic effect is due to inhibition of nerve conduction due to the blockade of sodium channels in nerve endings and nerve fibers. In its anesthetic effect, lidocaine is significantly (2-6 times) superior to procaine; the effect of lidocaine develops faster and lasts longer - up to 75 minutes, and when used simultaneously with epinephrine - more than 2 hours. When applied topically, it dilates blood vessels and does not have a locally irritating effect.
The antiarrhythmic properties of lidocaine are due to its ability to stabilize the cell membrane, block sodium channels, and increase membrane permeability for potassium ions. With virtually no effect on the electrophysiological state of the atria, lidocaine accelerates repolarization in the ventricles, inhibits the 4th phase of depolarization in Purkinje fibers (phase of diastolic depolarization), reducing their automaticity and the duration of the action potential, and increases the minimum potential difference at which myofibrils respond to premature stimulation. The rate of rapid depolarization (phase 0) is not affected or slightly reduced. It does not have a significant effect on the conductivity and contractility of the myocardium (it inhibits conductivity only in large, close to toxic doses). The PQ, QRS and QT intervals do not change under its influence on the ECG. The negative inotropic effect is also slightly expressed and appears short-term only with rapid administration of the drug in large doses.
Pharmacokinetics
Rapidly distributed in organs and tissues with good perfusion, incl. in the heart, lungs, liver, kidneys, then in muscle and adipose tissue. Penetrates the blood-brain and placental barriers and is secreted into breast milk (up to 40% of the concentration in maternal plasma). Metabolized mainly in the liver (90-95% of the dose) with the participation of microsomal enzymes with the formation of active metabolites - monoethylglycine xylidide and glycine xylidide. Excreted in bile and urine (up to 10% unchanged).
Indications
- infiltration, conduction, spinal and epidural anesthesia;
- terminal anesthesia (including in ophthalmology);
- relief and prevention of repeated ventricular fibrillation in acute coronary syndrome and repeated paroxysms of ventricular tachycardia (usually within 12-24 hours);
- ventricular arrhythmias caused by glycoside intoxication.
Release forms
Solution (injections in ampoules for injection and dilution).
Dosed spray (aerosol) 10%.
Eye drops 2%.
Gel or ointment 5%.
Instructions for use and dosage
For infiltration anesthesia: intradermal, subcutaneous, intramuscular. A lidocaine solution of 5 mg/ml is used (maximum dose 400 mg).
For blockade of peripheral nerves and nerve plexuses: perineurally, 10-20 ml of a 10 mg/ml solution or 5-10 ml of a 20 mg/ml solution (no more than 400 mg).
For conduction anesthesia: solutions of 10 mg/ml and 20 mg/ml (no more than 400 mg) are used perineurally.
For epidural anesthesia: epidural, solutions of 10 mg/ml or 20 mg/ml (not more than 300 mg).
For spinal anesthesia: subarachnoid, 3-4 ml of a solution of 20 mg/ml (60-80 mg).
In ophthalmology: a solution of 20 mg/ml is instilled into the conjunctival sac, 2 drops 2-3 times with an interval of 30-60 seconds, immediately before surgery or examination.
To prolong the action of lidocaine, it is possible to add extempore 0.1% adrenaline solution (1 drop per 5-10 ml of lidocaine solution, but no more than 5 drops for the entire volume of the solution).
As an antiarrhythmic agent: intravenously.
Lidocaine solution for intravenous administration 100 mg/ml can be used only after dilution.
25 ml of a 100 mg/ml solution should be diluted with 100 ml of saline to a lidocaine concentration of 20 mg/ml. This diluted solution is used to administer the loading dose. Administration begins with a loading dose of 1 mg/kg (over 2-4 minutes at a rate of 25-50 mg/min) with immediate continuation of a continuous infusion at a rate of 1-4 mg/min. Due to rapid distribution (T1/2 approximately 8 minutes), 10-20 minutes after the first dose, the concentration of the drug in the blood plasma decreases, which may require repeated bolus administration (against the background of continuous infusion) at a dose equal to 1/2-1/ 3 loading doses, with an interval of 8-10 minutes. The maximum dose in 1 hour is 300 mg, per day - 2000 mg.
The IV infusion is usually given over 12 to 24 hours with constant ECG monitoring, after which the infusion is stopped to assess the need for changes in the patient's antiarrhythmic therapy.
The rate of drug elimination is reduced in heart failure and liver dysfunction (cirrhosis, hepatitis) and in elderly patients, which requires a reduction in the dose and rate of drug administration by 25-50%.
For chronic renal failure, no dose adjustment is required.
Locally, by installation into the conjunctival sac immediately before examination or surgery, 1-2 drops. 2-3 times with an interval of 30-60 seconds.
The dose may vary depending on the indication and the size of the area to be anesthetized. One dose of the spray, released by pressing the dosing valve, contains 3.8 mg of lidocaine. To avoid achieving high concentrations of the drug in the blood plasma, the lowest doses at which a satisfactory effect is observed should be used. Usually 1-2 presses on the valve are sufficient, but in obstetric practice 15-20 or more doses are applied (the maximum number is 40 doses per 70 kg of body weight).
Side effect
- euphoria;
- headache;
- dizziness;
- drowsiness;
- general weakness;
- neurotic reactions;
- confusion or loss of consciousness;
- disorientation;
- convulsions;
- noise in ears;
- paresthesia;
- anxiety;
- decrease in blood pressure;
- chest pain;
- bradycardia (up to cardiac arrest);
- skin rash;
- hives;
- angioedema;
- anaphylactic shock;
- nausea, vomiting;
- feeling hot or cold;
- persistent anesthesia;
- erectile disfunction.
Contraindications
- sick sinus syndrome;
- severe bradycardia;
- 2-3 degree AV block (except when a probe is inserted to stimulate the ventricles);
- sinoatrial block;
- WPW syndrome;
- acute and chronic heart failure (3-4 FC);
- cardiogenic shock;
- pronounced decrease in blood pressure;
- Adams-Stokes syndrome;
- intraventricular conduction disorders;
- retrobulbar administration to patients with glaucoma;
- pregnancy;
- lactation period (penetrates the placental barrier, excreted in breast milk);
- hypersensitivity to any of the components of the drug.
Use during pregnancy and breastfeeding
Contraindicated for use during pregnancy and lactation.
Use in children
The drug should be used with caution in children.
special instructions
It is necessary to discontinue MAO inhibitors at least 10 days in case of planned use of lidocaine.
Caution should be exercised when performing local anesthesia in highly vascularized tissues; aspiration testing is recommended to avoid intravascular injection.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Drug interactions
Beta blockers and cimetidine increase the risk of toxic effects.
Reduces the cardiotonic effect of digitoxin.
Enhances muscle relaxation of curare-like drugs.
Aymaline, amiodarone, verapamil and quinidine enhance the negative inotropic effect.
Inducers of microsomal liver enzymes (barbiturates, phenytoin, rifampicin) reduce the effectiveness of lidocaine.
Vasoconstrictors (epinephrine, methoxamine, phenylephrine) prolong the local anesthetic effect of lidocaine and can cause increased blood pressure and tachycardia.
Lidocaine reduces the effect of antimyasthenic drugs.
Combined use with procainamide can cause central nervous system stimulation and hallucinations.
Guanadrel, guanethidine, mecamylamine, trimethaphan increase the risk of a pronounced decrease in blood pressure and bradycardia.
Strengthens and prolongs the effect of muscle relaxants.
The combined use of lidocaine and phenytoin should be used with caution, because it is possible to reduce the resorptive effect of lidocaine, as well as the development of an undesirable cardiodepressive effect.
Under the influence of MAO inhibitors, the local anesthetic effect of lidocaine and a decrease in blood pressure are likely to be enhanced. Patients taking MAO inhibitors should not be prescribed parenteral lidocaine.
When lidocaine and polymykisin B are prescribed simultaneously, it is necessary to monitor the patient's respiratory function.
When lidocaine is used in combination with hypnotics or sedatives, opioid analgesics, hexenal or sodium thiopental, the inhibitory effect on the central nervous system and respiration may be enhanced.
When lidocaine is administered intravenously to patients taking cimetidine, undesirable effects such as stunned state, drowsiness, bradycardia, and paresthesia are possible. This is due to an increase in the level of lidocaine in the blood plasma, which is explained by the release of lidocaine from its binding to blood proteins, as well as a slowdown in its inactivation in the liver. If combination therapy with these drugs is necessary, the dose of lidocaine should be reduced.
Instructions for use:
Lidocaine is a local anesthetic.
pharmachologic effect
Lidocaine is used for conduction, infiltration, and terminal anesthesia. The drug has a local anesthetic and antiarrhythmic effect.
As an anesthetic, the drug acts by inhibiting nerve conduction by blocking sodium channels in nerve fibers and endings. Lidocaine is significantly superior to procaine, its action occurs faster and lasts longer - up to 75 minutes (in combination with epinephrine - more than two hours). When applied topically, lidocaine dilates blood vessels and does not have a local irritating effect.
The antiarrhythmic effect of the drug is due to the ability to increase the permeability of membranes to potassium, block sodium channels, and stabilize cell membranes.
Lidocaine does not have a significant effect on myocardial contractility or conductivity (it affects only in large doses).
The level of absorption of Lidocaine when applied topically depends on the dosage of the product and the site of treatment (for example, Lidocaine is absorbed better on the mucous membranes than on the skin).
After intramuscular injections, Lidocaine reaches its maximum concentration 5-15 minutes after administration.
Release form
They produce Lidocaine spray, Lidocaine in ampoules (with solution for injections).
Indications for use of Lidocaine
Lidocaine 2% injections are used for local anesthesia in dentistry, surgery, ophthalmology, otolaryngology, for blocking nerve plexuses, peripheral nerves in patients with pain.
Lidocaine in 10% ampoules is used for anesthesia in the form of mucosal applications in ENT practice, gynecology, pulmonology, gastroenterology, dentistry during operations and diagnostic procedures. A 10% solution is also used as an antiarrhythmic agent.
Lidocaine spray is used in dentistry for removing baby teeth, tartar, fixing dental crowns, and performing other manipulations that require short anesthesia; in otolaryngology - for tonsillectomy, truncation of nasal polyps, septum, pain relief for the process of piercing and washing the maxillary sinus.
Lidocaine spray is effective during diagnostic procedures (insertion of a gastroduodenal tube, replacement of a tracheotomy tube) for anesthesia of the pharynx.
In gynecology, the spray is used to remove sutures, cut the female perineum during childbirth, and perform operations on the cervix.
In dermatology, the spray is used to anesthetize mucous membranes and skin during minor surgical procedures.
Contraindications
According to the instructions, lidocaine is contraindicated in cases of 2.3 degree atrioventricular block, 2.3 degree heart failure, severe bradycardia, arterial hypotension, cardiogenic shock, complete transverse heart block, porphyria, myasthenia, severe renal and hepatic pathologies, hypovolemia, glaucoma (for eye injections ), hypersensitivity, lactation, pregnancy.
Lidocaine spray is prescribed with caution to weakened, elderly patients, children, patients with epilepsy, in states of shock, with bradycardia, pathology of liver function, conduction disorders, pregnancy. During lactation, the spray can only be used in recommended dosages.
Instructions for use of Lidocaine
Before using Lidocaine, according to the instructions, you should conduct an allergy test to identify possible sensitivity to the drug. If swelling or redness occurs, lidocaine should not be used for anesthesia.
A solution of 2% Lidocaine (in ampoules) is intended for subcutaneous, intramuscular administration, conduction anesthesia, instillation into the conjunctival sac, and treatment of mucous membranes.
The dosage of the drug is individual, but the instructions for Lidocaine indicate the following average dosages: for conduction anesthesia, use 100-200 mg of the drug (no more than 200 mg), for anesthesia of the nose, ears, fingers - 40-60 mg of the drug.
When prescribing lidocaine injections, epinephrine is additionally prescribed to achieve the maximum therapeutic effect (if there are no contraindications).
In ophthalmology, up to six drops of solution are dripped, instilling two drops every 30-60 seconds. Usually 4-6 drops. enough for one eye for pain relief before operations and diagnostic procedures.
For terminal anesthesia, the maximum permissible dose of lidocaine according to the instructions is 20 ml. Treatment duration is 15-30 minutes.
When administering anesthesia to children, the total dosage should not exceed 3 mg per kg of child weight.
A solution of 10% Lidocaine (in ampoules) is administered intramuscularly and used in the form of applications. The permissible volume of Lidocaine for applications is 2 ml.
To stop an arrhythmic attack they do intramuscular injection Lidocaine – 200-400 mg. If the attack is not stopped, a second injection is given three hours later.
In case of arrhythmia, a 1.2% solution can be administered intravenously in a bolus - 50-100 mg, after which, according to the instructions, lidocaine is administered intramuscularly.
When using Lidocaine in ampoules of 2 and 10%, you should monitor the ECG and refrain from disinfecting the injection site with solutions containing heavy metals.
When prescribing the drug in high doses barbiturates are taken before the injection.
 Lidocaine spray is used only topically. Spray the drug from a short distance directly onto the area requiring pain relief, avoiding contact with the eyes and respiratory tract.
Lidocaine spray is used only topically. Spray the drug from a short distance directly onto the area requiring pain relief, avoiding contact with the eyes and respiratory tract.
When irrigating the oral cavity, due to decreased sensitivity, care should be taken not to injure the tongue with the teeth.
In dentistry and dermatology, 1-3 doses of 10% Lidocaine are used; in otolaryngology, craniofacial surgery – 1-4 doses of 10% Lidocaine; for endoscopic examination - 2-3 doses of 10% solution; in gynecology - 4-5 doses (while in obstetric practice, the use of up to 20 doses of a 10% solution is allowed).
When treating large areas, you can use a swab irrigated with lidocaine from a can.
Side effects
After the drug, weakness, headache, nystagmus, fatigue, euphoria, photophobia, hearing loss, numbness of the tongue, lips, drowsiness, nightmares, diplopia (double vision), cardiac rhythm and conduction disturbances, transverse heart block, decreased blood pressure may occur. chest pain, paresthesia, respiratory muscle paralysis, sensory disturbance, convulsions, tremor.
Lidocaine in large doses can lead to heart block, collapse, and cardiac arrest.
The drug can also cause shortness of breath, apnea, allergic rhinitis, conjunctivitis, dermatitis, dyspnea, urticaria, anaphylactic shock, nausea, vomiting, decreased body temperature, feeling hot, chills, numbness of the extremities, pain in the area where lidocaine injections were administered.
Lidocaine spray can provoke: burning sensation, allergic manifestations, low blood pressure, heart attack, depression, drowsiness, anxiety, loss of consciousness, spasms, paralysis respiratory tract, irritability





