Resuscitation - cardiac puncture
A myocardial puncture may be necessary during resuscitation to inject the drug directly into the ventricular cavity. More often, a puncture of the pericardial sac is used to aspirate (extract) fluid, blood in case of pericarditis and cardiac tamponade. The procedure is performed with a long needle under local anesthesia at special points. If the technique is followed, the puncture does not give serious complications.
Read in this article
When is a cardiac puncture needed?
An intracardiac injection of drugs may be required to restore the contractions of the heart during its sudden stop, an attack of arrhythmia that threatens life. Adrenaline, calcium chloride can be injected into the cavity of the ventricle. Due to the fact that this technique is effective in the first 3-7 minutes after clinical death, accompanied by the risk of damage to the coronary artery, bleeding, it is used relatively rarely.
Pericardial puncture is more common. It may be needed for the accumulation of blood or fluid in the pericardial sac in the following diseases:
- bleeding with, chest injury (), after a heart biopsy, probing, surgery, against the background of anticoagulant therapy;
- exfoliating;
- rupture of the wall with a heart attack;
- purulent, with tuberculosis, viral infections, bacterial damage;
- malignant neoplasms of the chest;
- severe degree of renal failure;
- complication of radiation therapy;
- autoimmune pathologies (, rheumatism);
- myxedema with insufficient thyroid function.
All indications can also be divided into emergency and planned. In the first case, the pericardial fluid compresses the heart, preventing its contractions. This state is called , and it leads to . And with planned manipulation, it is recommended to clarify the diagnosis, then the puncture is accompanied by an analysis of the resulting fluid to select the correct treatment.
It is not recommended to perform a planned puncture with a significant decrease in blood clotting activity, a drop in the platelet count in the blood, a recent coronary artery bypass grafting, and also if during the examination (X-ray or ultrasound) it is found that the cavity contains little fluid or it is not determined due to the fusion of the pericardial layers . With cardiac tamponade, puncture saves the patient's life, so contraindications are not taken into account.
The rate of fluid intake is important. A slow effusion into the pericardial cavity allows its leaves to gradually stretch and the volume of exudate reaches 1–2.5 liters, and with a sudden influx of 100–200 ml, compression of the heart and vena cava occurs.
This condition requires immediate puncture, as it threatens to stop contractions. Even when extracting 30-50 ml, the filling of the cardiac cavities improves, the stroke volume increases.
Methodology
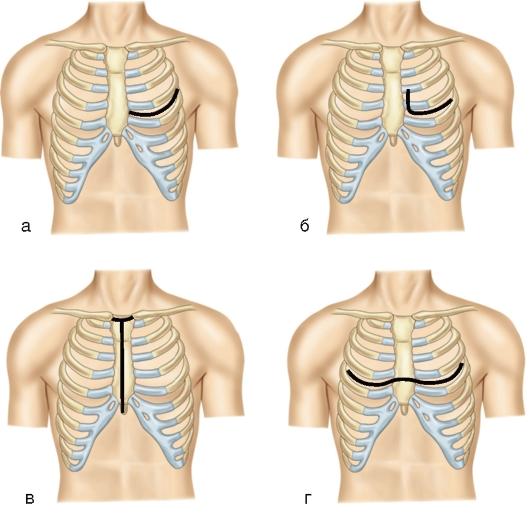
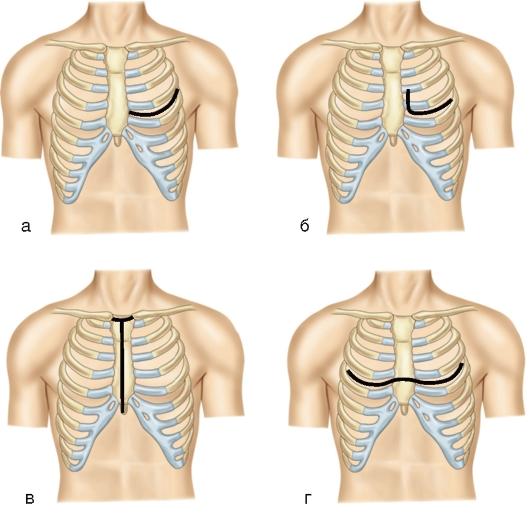
The puncture of the heart for the administration of medicines is carried out in the 4th left intercostal space, stepping back a finger thickness from the edge of the sternum. The needle is directed perpendicular to the front surface. When injected into the cavity of the heart, the syringe is freely filled with blood.
To puncture the pericardium, the patient should be in a horizontal position, a low pillow should be placed under the head, and a roller should be placed under the back at the border of the lower rib. Points are considered less dangerous areas for puncture:
- Larrey - the process of the sternum and the cartilaginous part of the costal arch (through the diaphragm);
- Marfana - the top of the xiphoid process;
- Pirogov - 4 - 5 intercostal space on the left edge of the sternum.
After treating the skin with an antiseptic, a local anesthetic is injected into the soft tissues. The skin, subcutaneous and muscular layer, tendon sheath is pierced at a right angle to a distance of about 2 cm. Then you need to change the direction to parallel to the surface of the chest, draw the needle up and back by about 25 - 30 mm.
If everything is done correctly, then there is a feeling of falling through, and the needle is in the pericardial bag and twitches a little when it comes into contact with its leaves.
Monitoring the work of the heart during puncture
In order to avoid damage to the heart during the puncture of the pericardium, it is necessary to constantly remove. If the needle is inside the cavity of the bag, then the ventricular complex remains unchanged. Possible complications are:
- deformation of the QRS complex, a decrease in its amplitude, the formation of pathological Q (the outer shell of the heart is affected);
- an increase in ST above the isoelectric line (the needle entered the myocardium), if it is tightened, then ST should return to normal;
- frequent atrial or ventricular extrasystoles, tachycardia attacks (may be at risk of heart puncture).
Monitoring can also be carried out with the help of echocardiography. It helps to detect the largest accumulation of fluid and accurately measure the distance that the needle can be inserted. After receiving the liquid, it is sent for analysis. If blood is found, then in order to find out its origin, a little content is left on a gauze napkin.
In case of traumatic injury during the puncture, the blood on the napkin will quickly clot, its color is scarlet, and in case of hemorrhagic pericarditis, it is absorbed, leaving only a pinkish trace.
Watch the video about pericardial puncture for cardiac tamponade:
Features of the needle for the procedure
For a puncture, a needle is needed, which has a length of about 10 cm and a diameter of 1.2 mm (size 18 - 21 G), most often used spinal. In order for it not to clog during penetration into the pericardial cavity, a thin wire is inserted into its lumen - a mandrin. After reaching the desired area of the pericardium, it is removed, and the fluid is aspirated.
If the fluid needs to be pumped out continuously (for example, progressive exudative pericarditis), then during the puncture, a 6 or 8 F catheter connected to the drainage system is inserted through the guidewire. It is usually firmly fixed on the skin.
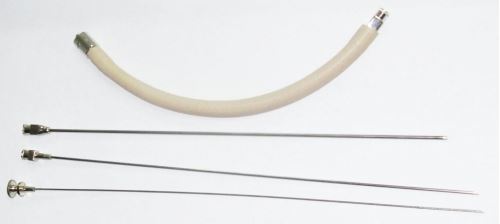
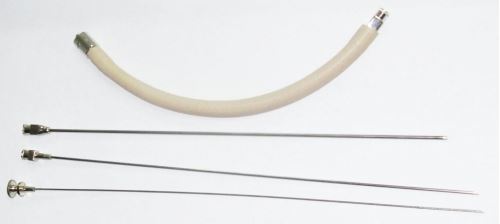 Needle for cardiac puncture (I-13)
Needle for cardiac puncture (I-13) Complications and their prevention
With careful observance of the pericardial puncture technique, complications rarely occur. However, during the procedure it is possible:
- heart injury;
- damage to arteries - internal thoracic or coronary;
- air vascular embolism;
- rhythm disturbance;
- injury to the pleura;
- fistula between the pleural and pericardial cavity;
- infection;
- sudden cardiac arrest.
Therefore, if the needle is likely to enter the cavity of the heart, it should be immediately removed, and the patient needs constant ECG and ultrasound monitoring to prevent bleeding. Direct access through the chest (thoracotomy) is necessary if the cardiogram data worsens or an air bubble blockage (embolism) of the vessel lumen is suspected.
 Operative access to the heart
Operative access to the heart Rhythm disturbances are removed with the help of either pacing,. If blood or air enters the pleural cavity, a puncture and installation of drains is performed. Signs of an inflammatory process require the appointment of antibiotic therapy.
Is it possible to pierce the heart with a puncture
With ECG and/or ultrasound monitoring of needle advancement, there is minimal risk of heart injury. However, when performing a heart puncture blindly, such a possibility is not excluded. The puncture of the pericardial sac in this case is performed for health reasons without the necessary equipment.
Injury to the myocardium of the left ventricle, as a rule, is not dangerous, since its high contractility helps to avoid bleeding. A more serious prognosis is possible if it enters the right ventricle, and especially the atrium. With such a complication, patients should be immediately hospitalized and monitored for at least a day in the intensive care unit.
Recovery after
After the end of the procedure, a chest X-ray, a control ECG and an ultrasound of the heart are indicated to exclude complications. If the patient's condition and examination data are normal, and there is no need for inpatient treatment, then the patient can be discharged home.
In the presence of a catheter, the place of its installation is treated with antiseptics, a bandage with an antibacterial ointment is applied. Dressings are carried out at least once every three days, the removal of fluid is recommended every 6 hours. If the daily volume is not more than 50 ml, then the catheter can be removed after control echocardiography. If the exudate acquires signs of a purulent process, then the catheter is removed, and the cavity is washed with an antiseptic, antibiotics are prescribed.
Cardiac puncture is performed to administer medications in intensive care. More often a puncture of the pericardial sac is shown to extract fluid. This may be a planned procedure for diagnosis or for health reasons in case of a threat of cardiac tamponade. Correct execution avoids serious complications. It is important during and after pericardial puncture to conduct an ECG and ultrasound of the heart, X-ray control of the state of the pleural and pericardial cavity.
Read also
If a person has pericarditis, surgery becomes the right decision. A heart puncture is performed to extract excess fluid and remove excess pericardial lobes, if necessary.








