Autoimmune thrombocytopenia ICD 10. Immune thrombocytopenia in children. Pregnancy and illness: symptoms
ICD-10 CODE
FANCONI ANEMIA
DIAMOND-BLACKFAN ANEMIA ICD-10 CODE
ICD-10 CODE
D61. Other aplastic anemias. Types of AA:
Congenital [Fanconi anemia (FA), Diamond-Blackfan anemia (DBA), dyskeratosis congenita, Shwachman-Diamond-Oski anemia, amegakaryocyte thrombocytopenia];
Acquired (idiopathic, caused by viruses, drugs or chemicals).
AA occurs with a frequency of 1-2 cases per 1,000,000 population per year and is considered a rare blood disease. Acquired AA develops with a frequency of 0.2-0.6 cases per 100,000 children per year. The average annual incidence rate of AA in children from 1979 to 1992 in the Republic of Belarus was 0.43±0.04 per 100,000 children. There were no differences in the incidence of AA in children before and after the Chernobyl disaster.
DBA is described under many names; partial red cell aplasia, congenital hypoplastic anemia, true erythrocyte anemia, primary red cell disease, erythrogenesis imperfecta. The disease is rare, L.K. Diamond et al. in the 60s XX century described only 30 cases of this disease; to date, more than 400 cases have been described.
Long time It was believed that the incidence of DBA is 1 case per 1,000,000 live newborns. In 1992, L. Wranne reported a higher incidence of 10 cases per 1,000,000 births. The incidence rate of DBA according to the French and English registries is 5-7 cases per 1,000,000 live newborns. The gender ratio is almost the same. More than 75% of DBA cases are sporadic; 25% are familial in nature, and in some families several patients are registered. The registry of patients with DBA in the USA and Canada includes 264 patients aged from 10 months to 44 years.
D61.0. Constitutional aplastic anemia.
FA is a rare autosomal recessive disorder characterized by multiple congenital physical anomalies, progressive bone marrow failure, and a predisposition to developing malignant neoplasms. The incidence of AF is 1 case per 360,000-3,000,000 population. The disease is common among all nationalities and ethnic groups. Minimum age of manifestation clinical signs- neonatal period™, maximum - 48 years. The register of patients with AF of the Research Institute of Pediatric Hematology of the Ministry of Health of the Russian Federation recorded the data of 69 patients. Average age manifestation of the disease - 7 years (2.5-12.5 years). 5 familial cases were identified.
HEMORRHAGIC DISEASES Purpura and other hemorrhagic conditions
D69.3. Idiopathic thrombocytopenic purpura.
Idiopathic thrombocytopenic purpura (ITP), according to many hematologists, is a common hemorrhagic disease. However, the only study in our country shows that the incidence rate of ITP in the Chelyabinsk region is 3.82 ± 1.38 cases per 100,000 children per year and does not have an increasing trend.
Idiopathic thrombocytopenic purpura (ITP)- a disease of unknown etiology, characterized by the development of thrombocytopenia and hemorrhagic syndrome. Most often, platelet destruction is caused by an autoimmune process provoked by an infectious agent or drug intake. Predominant age- up to 14 years old. Predominant gender- female.
Code by international classification diseases ICD-10:
- D69.3
Causes
Genetic aspects. Hereditary thrombocytopenic autoimmune idiopathic purpura has been described (188030, B), manifested by hemorrhagic syndrome, thrombocytopenia, and the presence of antibodies to platelets.
Classification. According to the course: acute (less than 6 months), chronic (more than 6 months). Periods of the disease.. Period of exacerbation (crisis).. Clinical remission.. Clinical and hematological remission. According to the clinical picture... Dry (isolated skin manifestations) .. Wet (addition of bleeding from the mucous membranes).
Clinical picture
. Acute onset with hemorrhagic syndrome. Body temperature may rise to subfebrile levels.
. The patient's condition often does not change significantly.
. Petechial - ecchymotic rash localized on the buttocks, inner thighs, chest, face.
. A positive pinch symptom is also possible in the stage of clinical remission.
. Bleeding from mucous membranes. The most common occurrence is intense nosebleeds; in girls of puberty - uterine bleeding.
. Internal bleeding in the gastrointestinal tract and central nervous system is extremely rare.
Laboratory research
. UAC: posthemorrhagic anemia, thrombocytopenia. OAM - possible hematuria due to renal bleeding. Immunogram: increase in CEC content. Myelogram: “irritation” of the megakaryocyte lineage, the appearance of “inactive” megakaryocytes.
Treatment
TREATMENT
Mode bed rest for severe thrombocytopenia.
Diet with the exception of obligate allergens.
Drug therapy
. For bleeding - etamsylate, aminocaproic acid, carbazochrome, hemostatic agents for local application, with intense nosebleeds - nasal tamponade. At uterine bleeding- oxytocin (as prescribed by the gynecologist).
. Antihistamines.
. Vitamin B15, Eleutherococcus.
. GC, for example prednisolone.. Indications - wet form of ITP, abundant skin manifestations on the face, scalp with platelet content less than 0.051012/l.. Prescribed in courses of 2-3 mg/kg/day for 5-7 days with breaks of 5-7 days.. Indication for cancellation is clinical and hematological remission by the first day of the next course.. If thrombocytopenia persists and there is no hemorrhagic syndrome, therapy is stopped after 4-5 courses.
. Inosine; orotic acid, potassium salt; lipoic acid.
. Immunosuppressive therapy - effectiveness is questionable.
. Alternative drugs. Recombinant IFN preparations for chronic course.. Induction: 3 million units/m2 3 times/week. The duration of the course depends on the “response” (recovery period and platelet count). Maintenance therapy for 12 weeks.
. Intravenous infusions IgG is new and effective method, which helps increase the number of platelets during an acute attack. ATs block Fc receptors of phagocytes, which play an important role in antiplatelet cytotoxic reactions; this method has gained popularity as a preoperative preparation for patients with ITP who require surgical intervention. A new method of treating refractory ITP, which has given encouraging results preliminary results, - plasmapheresis through a column with staphylococcal proteins.
Surgical treatment. Splenectomy is indicated for chronic form with severe bleeding with unsuccessful conservative therapy. Cure with splenectomy does not always occur. Occlusion of splenic vessels.
Observation. In the stage of clinical remission - control of platelet levels 1 time per month. If clinical and hematological remission lasts more than 5 years, the patient is removed from the register.
Recommendations. Observation by a hematologist at the place of residence. Physiotherapeutic treatment and insolation are contraindicated. Use is contraindicated acetylsalicylic acid, carbenicillin. Prevention of bleeding - herbal medicine (infusions of chamomile, nettle, rosehip) in courses of 15 days every 3 months. Physical education and sports should be avoided. Registration of disability in case of persistent chronic disease.
Complications. Hemorrhages in the central nervous system. Severe posthemorrhagic anemia.
Course and prognosis. In most patients (80-90%), self-healing occurs within 1-6 months. When the process is chronic, the treatment regimen with prednisolone is similar. The mortality rate for ITP is less than 1%. Causes of death- hemorrhages in the central nervous system, severe posthemorrhagic anemia.
Reduction. ITP - idiopathic thrombocytopenic purpura
ICD-10. D69.3 Idiopathic thrombocytopenic purpura
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Clinical protocols Ministry of Health of the Republic of Kazakhstan - 2016
Idiopathic thrombocytopenic purpura (D69.3)
Children's Oncology, Pediatrics
general information
Short description
Approved
Joint Commission on Quality medical services
Ministry of Health and social development Republic of Kazakhstan
dated November 29, 2016
Protocol No. 16
Immune thrombocytopenia - autoimmune disease, characterized by isolated thrombocytopenia (less than 100,000/μl) with a constant/increased number of megakaryocytes in the bone marrow and the presence of antiplatelet antibodies on the surface of blood platelets and in the plasma of patients, usually acting on membrane glycoprotein complexes IIb/IIIa and/or GPIb/IX, which leads to the destruction of platelets by cells of the phagocytic mononuclear cell system, manifested by hemorrhagic syndrome.
Correlation of ICD-10 and ICD-9 codes
| ICD-10 | ICD-9 | ||
| Code | Name | Code | Name |
| D69.3 | immune thrombocytopenia | - | - |
Date of development of the protocol: 2016
Protocol users: GPs, therapists, cardiologists, hematologists, pediatricians, oncologists.
Level of evidence scale
| A | A high-quality meta-analysis, systematic review of RCTs, or large RCTs with a very low probability (++) of bias, the results of which can be generalized to an appropriate population. |
| IN | High-quality (++) systematic review of cohort or case-control studies or High-quality (++) cohort or case-control studies with very low risk bias or RCTs with a low (+) risk of bias, the results of which can be generalized to the appropriate population. |
| WITH |
Cohort or case-control study or controlled trial without randomization with low risk of bias (+). The results of which can be generalized to the relevant population or RCTs with very low or low risk of bias (++ or +), the results of which cannot be directly generalized to the relevant population. |
| D | Case series or uncontrolled study or expert opinion. |
Classification
ClassificationAmerican Society of Hematology, 2013:
With the flow:
· newly identified - duration up to 3 months;
· persistent (protracted) ITP - duration 3-12 months;
Chronic ITP - duration more than 12 months.
According to the severity of hemorrhagic syndrome:
· severe - patients with clinically significant bleeding, regardless of platelet level. Cases accompanied by symptoms of bleeding at the onset of the disease, requiring initiation of therapy, or cases of resumption of bleeding with the need for additional therapeutic benefits different drugs, increasing the platelet count, or increasing the dosage used medicines.
· refractory - inability to obtain a response or a complete response (platelets less than 30x109/l) to therapy after splenectomy; loss of response after splenectomy and need drug treatment in order to minimize clinically significant bleeding. In this case, a repeat examination is required to exclude other causes of thrombocytopenia and confirm the diagnosis of ITP. Mainly found in adults.
By stages; Standardization of ITP, Sept 2006 IMBACH]:

Diagnostics (outpatient clinic)
OUTPATIENT DIAGNOSTICS
Diagnostic criteria: NB! Primary immune thrombocytopenia is diagnosed when platelets decrease to less than 100x109/l, with the exclusion of other causes of thrombocytopenia.
Diagnostic criteria for diagnosis:
Complaints:
increased bleeding from mucous membranes;
Anamnesis:
· nosebleeds, gum bleeding;
· menorrhagia, metrorrhagia;
· hemorrhages in the sclera;
· hemorrhages in the brain;
· hematuria;
· bleeding from the gastrointestinal tract (bloody vomiting, melena);
· hemorrhagic rashes in the form of petechiae and ecchymoses on the skin.
Physical examination:
General inspection:
Character of cutaneous hemorrhagic syndrome:
· location and size of petechiae and bruises;
· presence of hemorrhages on the oral mucosa, conjunctivae;
blood flowing down back wall pharynx;
· anomalies of the structure of the face (triangular face, small eyes, epicanthus, small facial features) and limbs (anomalies of the 1st finger of the hands, six-fingered, syndactyly, clinodactyly);
Laboratory research:
· UAC with manual counting leukocyte formula and platelet morphology - in the hemogram isolated thrombocytopenia is noted - a decrease in platelets less than 100x10 9 / l without changes in leukocyte and erythrogram parameters. In some cases, posthemorrhagic anemia and changes in the leukogram associated with concomitant infectious disease, allergies;
No.
Diagnostic algorithm at the outpatient level:

Diagnostics (hospital)
DIAGNOSTICS AT THE INPATIENT LEVEL
Diagnostic criteria:
Complaints: see outpatient level.
Anamnesis:
Duration and nature of bleeding;
· vaccination (especially combined vaccination against measles, mumps and rubella) 2-3 weeks before the development of hemorrhagic syndrome;
· transferred (respiratory viral, rubella, infectious mononucleosis) 2-3 weeks before the development of hemorrhagic syndrome;
· use of medications (in particular heparin) during the last 2-3 weeks;
presence of bone pain and weight loss;
Physical examination: see outpatient level .
Laboratory research:
· UAC with manual calculation of the leukocyte formula and platelet morphology - the hemogram shows isolated thrombocytopenia - a decrease in platelets less than 100x109/l without changing the leukocyte and erythrogram values. In some cases, posthemorrhagic anemia and changes in the leukogram associated with a concomitant infectious disease or allergy may be recorded;
Instrumental studies: No.
Diagnostic algorithm at the stationary level: No.

List of main diagnostic measures carried out at the stationary level:
· CBC (counting platelets and reticulocytes in a smear);
· blood type and Rh factor;
· biochemical blood test (protein, albumin, ALT, ACaT, bilirubin, creatinine, urea, dextrose);
· myelogram: hyperplasia of the megakaryocyte lineage with the appearance of young generations of megakaocytes and an increased content of their precursors;
· duration of bleeding according to Sukharev;
· OAM;
· ELISA for markers of viral hepatitis (HbsAg);
· ELISA for markers of viral hepatitis HCV;
· ELISA for HIV markers.
List of additional diagnostic examinations carried out at the stationary level:
· biochemical analysis: GGTP, electrolytes;
· coagulogram;
· ELISA for antithrombotic antibodies;
Immunophenotyping of peripheral blood cells;
· immunogram;
· antiphospholipid antibodies;
PCR for viral infections (viral hepatitis, cytomegalovirus, virus herpes simplex, Epstein-Barr virus, Varicella/Zoster virus);
· echocardiography;
· Ultrasound of organs abdominal cavity(liver, spleen, pancreas, gallbladder, lymph nodes, kidneys), mediastinum, retroperitoneum and pelvis - to exclude hemorrhage in internal organs;
· CT scan brain: carried out if there is suspicion of intracranial hemorrhage - headache, vomiting, paresis, disturbances of consciousness; to exclude stroke;
· Ultrasound of OBP.
Differential diagnosis
| Diagnosis | Rationale for differential diagnosis | Survey | Diagnosis exclusion criteria |
| TAR syndrome | Characterized by pathology of megakaryocytes and platelets with their hypoplasia and dysfunction, which leads to bleeding | Collection of complaints and anamnesis, physical examination method. | Characterized by the absence radius, congenital pathology megakaryocytes and platelets with their hypoplasia and dysfunction, which leads to bleeding. Children get sick most often accompanied by congenital anomalies organs (often heart defects) |
| Aplastic anemia | In blood smears, isolated thrombocytopenia is often deep until single blood platelets are detected. | CBC with counting of leukocyte formula, reticulocytes. Myelogram, trephine biopsy. | Bone marrow aspirate is poor in nuclear elements. Reduced total percentage cellular elements. In histological preparations of trephine biopsy specimens of the iliac bones, bone marrow aplasia with replacement of adipose tissue excludes ITP. Iron levels are normal or elevated. |
| Myelodysplastic syndrome | Hemorrhagic syndrome | CBC (with leukocyte count, reticulocyte count). Myelogram, trephine biopsy. | MDS is characterized by signs of dyspoiesis, an excess of blasts in the bone marrow, chromosomal aberrations, which excludes ITP |
| Hematoblastoses | Pancytopenia, hemorrhagic syndrome | CBC (with leukocyte count, reticulocyte count). Myelogram. | Results of flow cytometry, immunohistochemical, histological examination bone marrow excludes ITP. |
| Paroxysmal nocturnal hemoglobinuria | Hemorrhagic syndrome |
UAC; Blood chemistry; Coagulogram; OAM; IFT on PNG. |
PNH is characterized by hemosiderinuria, hemoglobinuria, increased levels of bilirubin, LDH, and a decrease or absence of haptoglobin. Bleeding is rarely observed; hypercoagulation (activation of aggregation inducers) is typical. Excluded if there is no PNH clone based on IFT results. |
| Megaloblastic anemia. | thrombocytopenia |
CBC + peripheral blood morphology; Myelogram; Biochemical blood test (cyanocobalamin and folic acid levels). |
Indirect signs characteristic of megaloblastic anemia are an increase in the average hemoglobin content in erythrocytes, an increase in the average volume of erythrocytes, and the megaloblastic type of hematopoiesis according to the myelogram. Unlike ITP, in megaloblastic anemia, despite thrombocytopenia, there is no hemorrhagic syndrome. |
| Thrombotic thrombocytopenic purpura. | Hemorrhagic syndrome |
UAC; Ultrasound of OBP; Assessment of neurological status; X-ray of joints. |
It is excluded on the basis of neurological symptoms, the formation of multiple blood clots, articular syndrome, and often enlargement of the liver and spleen. |
Treatment abroad
Get treatment in Korea, Israel, Germany, USA
Get advice on medical tourism
Treatment
Drugs ( active ingredients), used in the treatment
| Hemostatic sponge |
| Azithromycin |
| Alemtuzumab |
| Amoxicillin |
| Acyclovir |
| Dexamethasone |
| Immunoglobulin G human normal (Immunoglobulin G human normal) |
| Captopril |
| Clavulanic acid |
| Kolekaltsiferol |
| Platelet concentrate (CT) |
| Mycophenolic acid (Mycophenolate mofetil) |
| Omeprazole |
| Pancreatin |
| Paracetamol |
| Piperacillin |
| Prednisolone |
| Rituximab |
| Tazobactam |
| Tranexamic acid |
| Thrombinum |
| Fluconazole |
| Ceftazidime |
| Cyclosporine |
| Cyclophosphamide |
| Eltrombopag |
| Etamsylate |
Treatment (outpatient clinic)
OUTPATIENT TREATMENT
Treatment tactics: No.
− Non-drug treatment: No.
− Drug treatment: No.
Algorithm of action in emergency situations: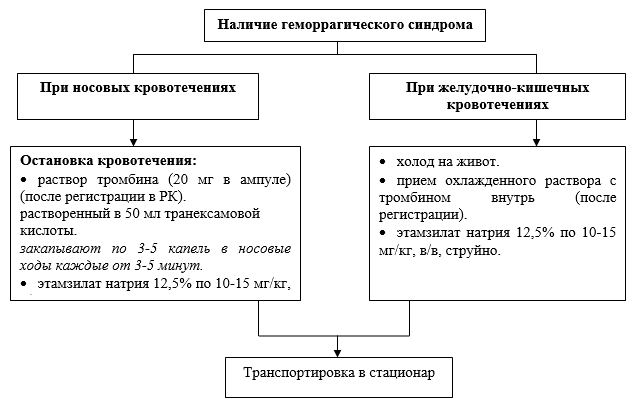
· consultation with an oncohematologist - if hematoblastosis is suspected;
· consultation with a gynecologist - for metrorrhagia, menorrhagia;
Treatment (ambulance)
DIAGNOSIS AND TREATMENT AT THE EMERGENCY CARE STAGE
Diagnostic measures:
· collection of complaints and medical history;
· physical examination.
Drug treatment:
· symptomatic therapy ,
according to IMCI - WHO guidelines for the management of the most common diseases in primary level hospitals, adapted to the conditions of the Republic of Kazakhstan.
Treatment (inpatient)
INPATIENT TREATMENT
Treatment tactics:
For immune thrombocytopenia, treatment tactics begin with the prescription of a hormonal drug (prednisolone). With a favorable response to treatment, the platelet count increases (usually on days 7-10) and remains stable for high level even after discontinuation of the drug. If remission does not occur, immunotherapy is prescribed - intravenous immunoglobulin. If it is not possible to bring the patient into remission with drug therapy within 6 months, splenectomy is recommended. In severe cases of the disease, splenectomy can be performed at an earlier date.
To decide on treatment tactics, international group experts developed a bleeding scale and recommendations on the approach
to therapy:
| Bleeding/quality of life | Therapeutic approach |
|
Degree 1. Minor bleeding<100 петехий и/или < 5 мелких синяков (<3 см в диаметре); отсутствие кровоточивости слизистых |
Observation |
|
Degree 2. Light bleeding. Multiple petechiae > 100; and/or >5 large bruises (>3 cm in diameter); no bleeding of mucous membranes |
Observation or, in some patients, membrane stabilizing therapy |
|
Degree 3. Moderate bleeding. The presence of bleeding of mucous membranes, a “dangerous” lifestyle |
Consultation with a hematologist |
|
Degree 4. Bleeding of mucous membranes or suspicion of internal bleeding |
Treatment of all patients in a hospital setting |
Non-drug treatment:
Mode: II.III;
Diet: № 11.
Drug treatment
Treatment depending on severity:
Use standard dose of prednisolone for a maximum of 14 days/increased dose for 4 days
First-line treatment for ITP:
| Drugs | Dose | Duration of therapy |
UD, link |
| Prednisolone | 0.25 mg/kg | 21 days | Grade A |
| 2 mg/kg | 14 days with gradual withdrawal | ||
| 60 mg/m 2 | 21 days | ||
| 4mg/kg | 7 days with gradual withdrawal | ||
| 4mg/kg | 4 days | ||
| Methylprednisolone | 30 or 50 mg/kg | 7 days | Grade A |
| 20-30mg/kg | 2 - 7 days | ||
| 30mg/kg | 3 days | ||
| IVIG | 0.8-1 g/kg | 1-2 days | Grade A |
| 0.25 g/kg | One time | ||
| 0.4 g/kg | 5 days | ||
| Anti-D | 25µg/kg | 2 days | Grade A |
| 50-60mcg/kg | One time | ||
| 75mcg/kg | One time | ||
| Dexamethasone | 20 - 40 mg/kg/day | for 4 consecutive days (every month, 6 cycles) | Grade A |
Persistent and chronic ITP:
glucocorticoid therapy regimens: high doses methylprednisolone IV 30 mg/kg x 3 days, then 20 mg/kg x 4 days;
· IVIT can also be used for CITP, before surgical interventions, tooth extraction/in case of injury. The regimens for using IVIT for cITP are identical to those for new-onset ITP;
· recommended dose of IVIT is 0.8-1.0 g/kg body weight followed by reintroduction within 48 hours, if after the first administration the platelet level is not higher than 20 x 109/l.
Drug therapy second line:
Rituximab(UD-B):
· single dose: 375 mg/m2/week, course duration: 4 weeks (4 injections in total);
Indications:
· non-responders to high doses of dexamethasone;
· if there are contraindications to splenectomy;
· recurrent and refractory course of ITP.
Cyclosporine A:
· 2.5 - 3 mg/kg/day. In combination with Prednisolone (UD-B)
Cyclophosphamide: 200 mg/m2 1 time per day;
Indications:
· in patients resistant to hormone therapy and/or after splenectomy;
· secondary ITP.
Mycophenolate mofetin: 20-40 mg/kg, course duration 30 days.
Indications:
· some patients with antiproliferative and immunosuppressive purposes.
Third line drug therapy:
TPO receptor agonists(UD-A):
· Eltrombopag 25-75 mg orally 1-10 mg/kg/week.
Alemtuzumab*:
· alternative therapy for cITP and refractory ITP.NB! used against the background of accompanying therapy (antibacterial, antifungal, antiviral).
List of essential medicines:
| INN of the drug | Release form |
UD, link |
| Immunosuppressive drugs | ||
| dexamethasone |
tablets 0.5 mg solution 4 mg/2 ml |
UD B |
| prednisolone | 5 mg tablets | UD A |
| for intravenous administration 10% 2 g/20 ml | UD A | |
| immunoglobulin human Ig G | for intravenous administration 10% 5 g/50 ml | UD A |
| cyclophosphamide | powder for the preparation of solution for intravenous administration 500 mg | UD S |
| mycophenolate mofetil | capsules 250 and 500 mg | UD S |
| rituximab |
bottles 10 ml/100 mg bottles 50 ml/500 mg |
UD B |
| cyclosporine A | capsules 25 mg, 50 mg, 100 mg | UD B |
| Eltrombopag | tablets 31.9 mg and 63.8 mg | UD A |
| Alemtuzimab (after registration in the Republic of Kazakhstan) | solution for infusion 1ml | UD A |
| Antifungal drugs(according to indications) | ||
| fluconazole | solution for intravenous injection, 50 ml, 2 mg/ml, capsules 150 mg | UD B |
| Antimicrobials used to prevent the development of purulent-septic complications, as well as after determining sensitivity to antibiotics | ||
|
azithromycin or |
tablet/capsule, 500 mg, lyophilized powder for the preparation of solution for intravenous infusion, 500 mg; | UD B |
|
piperacillin/tazobactam or |
powder for the preparation of injection solution for intravenous administration 4.5 g | UD B |
|
ceftazidime or |
powder for the preparation of injection solution for intravenous administration 1000 mg | UD B |
| amoxocillin + clavulanic acid |
tablet coated film-coated, 500 mg/125 mg, powder for the preparation of suspension for oral administration 135 mg/5ml, powder for the preparation of a solution for intravenous and intramuscular administration 600 mg. |
UD B |
| Antiviral ( according to indications, in cases of infection) | ||
| acyclovir | cream for external use 5% -5.0, tablet 200 mg, powder for solution for infusion 250 mg; | UD S |
| Medicines affecting the blood coagulation system | ||
| fibrinogen+thrombin | hemostatic sponge, size 7*5*1, 8*3; | UD B |
List of additional medicines:
| INN of the drug |
Route of administration |
UD, link |
| omeprazole (prevention of antiulcer therapy) | for oral administration 20 mg | UD B |
| pancreatin (for gastritis, improves the digestion process with hormone therapy) | 10000 IU | UD B |
| captopril (for increased blood pressure) | tablet for oral administration 12.5 mg | UD B |
| paracetamol (antipyretic) | tablet for oral administration 200 mg | UD B |
| sodium ethamsylate (for bleeding) |
for oral administration for intravenous administration 2 ml |
UD B |
| colecalciferol (for hypocalcemia) | 500 mg tablets | UD B |
Use of platelet concentrate transfusions:
Indications:
· presence of life-threatening bleeding.
Transfusions of platelet concentrate should always complement specific therapy for ITP (IVIG and/or glucocorticoids) and should not be used as monotherapy. If the severity of bleeding in ITP is such that it requires transfusion of platelet concentrate, split transfusions are recommended - every 6-8 hours. In especially severe cases, “hyperfractionated” transfusions with small doses of platelet concentrate are used: 1-2 doses (0.7-1.4x10 11) every two hours. Etamsylate and antifibrinolytic drugs are used as additional hemostatic therapy.
NB! In case of renal bleeding, the administration of fibrinolysis inhibitors is contraindicated.
Surgical intervention:
Splenectomy(UD-B)
Indications for intervention:
· recurrent, severe course of the disease for more than 6 months;
· patients over 6 years of age after prior vaccination with Haemophilus influenzae type b + S.pneumoniae + N.Meningitidis.
Contraindications for intervention:
· children under 6 years old;
· primary ITP.
Other treatments: No.
Auxiliary hemostatic therapy:
· sodium ethamsylate 12.5% at a dose of 10-15 mg/kg;
· para-aminobenzoic acid - tranexamic acid: over the age of 12 years at a dose of 20-25 mg/kg.
Indications for consultation with specialists:
· consultation with an infectious disease specialist - if an infectious process is suspected;
· consultation with an endocrinologist - if endocrine disorders develop during treatment;
· consultation with an obstetrician-gynecologist - during pregnancy, metrorrhagia, menorrhagia, when prescribing combined oral contraceptives;
· consultation with other narrow specialists - according to indications.
Indications for transfer to the intensive care unit:
· absence/impaired consciousness (Glasgow scale); application No. 1
acute cardiovascular failure (heart rate less than 60, or more than 200 per minute);
· acute respiratory failure (difficulty of breathing 2 - 3 degrees, respiratory rate more than 50, decreased saturation less than 88%, the need for mechanical ventilation);
acute circulatory disorder ( states of shock);
· Systolic blood pressure, less than 60/more than 180 (requiring constant administration of vasoactive drugs);
· critical metabolic disorders (electrolyte, water, protein, acid-base balance, ketoacidosis);
· intensive observation and intensive pharmacotherapy, requiring constant monitoring of vital functions;
· violation of blood coagulation and anticoagulation systems.
Indicators of treatment effectiveness:
· after 4 weeks from the start of treatment, an increase in platelets above 100x10 9 / l (75% of patients with ITP).
· after removal of the spleen - an increase in the level of platelets in the peripheral blood.
Further management
Laboratory research:
· A CBC with determination of the platelet count and manual counting of the leukocyte formula (mandatory) is carried out once a month in the first year of observation. Further depending on clinical condition and stability of the hematological picture;
· dynamic biochemical blood analysis is carried out if indicated;
· serological testing of markers of HIV, hepatitis B and C, carried out 3 months after discharge from the hospital and 3 months after each transfusion of blood products.
Condition for transferring the patient to the place of residence:
· pediatrician (pediatric hematologist) at the place of residence is guided by the recommendations given by hospital specialists;
· the frequency of examination of a patient with ITP is once every 2-4 weeks in the first 3 months of treatment, then depending on the clinical condition and hematological dynamics, but at least once every 2 months.
Instrumental studies carried out when clinically indicated.
Hospitalization
Indications for planned hospitalization:
Indications for emergency hospitalization:
Decrease in platelet level in CBC<50х10 9 /л.
· presence of hemorrhagic syndrome (bleeding from the mucous membranes of the nasopharynx, oral cavity, gastrointestinal bleeding, uterine bleeding).
Information
Sources and literature
- Minutes of meetings of the Joint Commission on the Quality of Medical Services of the Ministry of Health of the Republic of Kazakhstan, 2016
- 1) Pediatric hematology, 2015. Edited by A.G. Rumyantsev, A.A. Maschan, E.V. Zhukovskaya. Moscow. Publishing group "GEOTAR-Media" 2015 C – 656, C-251, table 6. 2) The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia Cindy Neunert, Wendy Lim, Mark Crowther, Alan Cohen, Lawrence Solberg, Jr and Mark A. Crowther2011; 16:4198-4204 3) Standardization of ITP, Sept 2006 IMBACH. 4) Providing emergency care, 2005. Algorithm of actions in emergency situations: according to IMCI - WHO guidelines for the management of the most common diseases in primary level hospitals, adapted to the conditions of the Republic of Kazakhstan (WHO 2012). 5) ESH. The Handbook "Immune thrombocytopenia" 2011. 6) Tarantino & Buchanan, Hematol Oncol Clin North Am, 2004, 18:1301-1314. 7) Guidelines for the adminis parenteral nutrition Canada 2010. 8) SIGN 104. Antibiotic prophylaxis in surgery.2014.
Information
Abbreviations used in the protocol
| AG | arterial hypertension; |
| HELL | arterial pressure; |
| ALaT | alanine aminotransferase |
| ASa T | aspartate aminotransferase |
| IV | intravenously |
| i/m | intramuscularly |
| VVID | intravenous high-dose immunoglobulin therapy |
| HIV | AIDS virus; |
| GGTP | gammaglutamyl transpeptidase; |
| IMCI | integrated management of childhood illnesses |
| mechanical ventilation | artificial ventilation |
| AND SO ON | immune thrombocytopenia |
| ELISA | linked immunosorbent assay; |
| IFT | immunophenotyping; |
| CT | CT scan; |
| KSH | acid-base state |
| LDH | lactate dehydrogenase; |
| Health care facilities | medical institution |
| MDS | myelodysplastic syndrome; |
| ME | international units |
| MMF | mycophenolate mofetin |
| MRI | Magnetic resonance imaging |
| UAC | general blood analysis |
| OAM | general urine analysis; |
|
AML PNG |
acute myeloblastic leukemia; paroxysmal nocturnal hemoglobinuria; |
| ONMK | acute cerebrovascular accident |
| PCR | polymerase chain reaction; |
| ESR | - erythrocyte sedimentation rate; |
| HSCT | hematopoietic stem cell transplantation |
| USDG | Doppler ultrasound |
| FGDS | fibro-gastro-duadenoscopy |
| hITP | chronic immune thrombocytopenia |
| CMV | cytomegalovirus |
| BH | breathing rate; |
| Heart rate | heart rate; |
| ECG | electrocardiography; |
| EchoCG | echocardiography; |
| Ig | immunoglobulin |
List of protocol developers with qualification information:
1) Omarova Gulnara Erbosynovna - pediatric hematologist/oncologist, Branch of the Corporate Foundation "UMC", "National Scientific Center for Maternity and Childhood", Astana.
2) Tastanbekova Venera Bulatovna - pediatric hematologist/oncologist, Branch of the Corporate Foundation “UMC”, “National Scientific Center for Maternity and Childhood”, Astana.
3) Umirbekova Balzhan Bolatovna - pediatric hematologist/oncologist, Branch of the Corporate Foundation "UMC", "National Scientific Center for Maternity and Childhood", Astana.
4) Omarova Kulyan Omarovna - Doctor of Medical Sciences, Professor, National Center for Pediatrics and Children's Surgery, Almaty.
5) Manzhuova Lyazzat Nurpapaevna - Candidate of Medical Sciences, Head of Oncology Department No. 1, National Center of Pediatrics and Children's Surgery, Almaty.
6) Mira Maratovna Kalieva - Candidate of Medical Sciences, Associate Professor of the Department of Clinical Pharmacology and Pharmacotherapy of KazNMU named after. S. Asfendiyarova.
Indication of no conflicts: No.
List of reviewers: Kemaykin Vadim Matveevich - hematologist of the highest qualification category, candidate of medical sciences, chief freelance hematologist, oncohematologist of the Ministry of Health and Social Development of the Republic of Kazakhstan.
Annex 1

Attached files
Attention!
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Guide" cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications "MedElement", "Lekar Pro", "Dariger Pro", "Diseases: Therapist's Directory" are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
The disease begins gradually or acutely with the appearance of hemorrhagic syndrome. The type of bleeding in thrombocytopenic purpura is petechial-spotted (bruised). According to clinical manifestations, two variants of thrombocytopenic purpura are distinguished: “dry” - the patient experiences only cutaneous hemorrhagic syndrome; “wet” - hemorrhages combined with bleeding. Pathognomonic symptoms of thrombocytopenic purpura are hemorrhages in the skin, mucous membranes and bleeding. The absence of these signs raises doubts about the correctness of the diagnosis.
Cutaneous hemorrhagic syndrome occurs in 100% of patients. The number of ecchymoses varies from single to multiple. The main characteristics of cutaneous hemorrhagic syndrome in thrombocytopenic purpura are as follows.
- Inconsistency between the severity of hemorrhage and the degree of traumatic exposure; their spontaneous appearance is possible (mainly at night).
-Polymorphism of hemorrhagic rashes (from petechiae to large hemorrhages).
-Polychrome skin hemorrhages (color from purple to blue-greenish and yellow depending on how long ago they appeared), which is associated with the gradual conversion of hemoglobin through intermediate stages of decomposition into bilirubin.
-Asymmetry (no favorite localization) of hemorrhagic elements.
- Painless.
Hemorrhages often occur in the mucous membranes, most often the tonsils, soft and hard palate. Hemorrhages into the eardrum, sclera, vitreous body, and fundus are possible.
Hemorrhage into the sclera may indicate a threat of the most severe and dangerous complication of thrombocytopenic purpura - hemorrhage in the brain. As a rule, it occurs suddenly and progresses quickly. Clinically, cerebral hemorrhage is manifested by headache, dizziness, convulsions, vomiting, and focal neurological symptoms. The outcome of cerebral hemorrhage depends on the volume, localization of the pathological process, timely diagnosis and adequate therapy.
Thrombocytopenic purpura is characterized by bleeding from the mucous membranes. They are often profuse in nature, causing severe posthemorrhagic anemia, which threatens the patient’s life. In children, bleeding most often occurs from the nasal mucosa. Bleeding from the gums is usually less profuse, but it can also become dangerous during tooth extraction, especially in patients with an undiagnosed disease. Bleeding after tooth extraction in thrombocytopenic purpura occurs immediately after the intervention and does not resume after its cessation, unlike late, delayed bleeding in hemophilia. In girls of puberty, severe menorrhagia and metrorrhagia are possible. Gastrointestinal and renal bleeding occur less frequently.
There are no characteristic changes in internal organs with thrombocytopenic purpura. Body temperature is usually normal. Sometimes tachycardia is detected, during auscultation of the heart - systolic murmur at the apex and at Botkin's point, weakening of the first tone, caused by anemia. An enlarged spleen is uncharacteristic and rather excludes the diagnosis of thrombocytopenic purpura.
According to the course, acute (lasting up to 6 months) and chronic (lasting more than 6 months) forms of the disease are distinguished. During the initial examination, it is impossible to determine the nature of the course of the disease. Depending on the degree of manifestation of the hemorrhagic syndrome and blood parameters during the disease, three periods are distinguished: hemorrhagic crisis, clinical remission and clinical-hematological remission.
Hemorrhagic crisis is characterized by severe bleeding syndrome and significant changes in laboratory parameters.
During clinical remission, hemorrhagic syndrome disappears, bleeding time is reduced, secondary changes in the blood coagulation system are reduced, but thrombocytopenia persists, although it is less pronounced than during a hemorrhagic crisis.
Clinical and hematological remission implies not only the absence of bleeding, but also the normalization of laboratory parameters.





